
The
Diagnostic
Importance
of
the
History
and
Physical
Examination
as
Determined
by
the
Use
of
a
Medical
Decision
Support
System
Michael
M.
Wagner,
M.D.,
Richard
A.
Bankowitz,
M.D.,
Melissa
McNeil,
M.D.*
Susan
M.
Challinor,
M.D.*,
Janine
E.
Janosky,
Ph.D.**,
Randolph
A.
Miller,
M.D.
Section
of
Medical
Informatics,
University
of
Pittsburgh
School
of
Medicine
*Veterans
Administration
Medical
Center,
Pittsburgh
**Departrnent
of
Clinical
Epidemiology
and
Preventive
Medicine
Abstract
Automated
analysis
of
NEJM
CPC
cases
was
used
to
assess
the
relative
importance
of
history
and
physical
examination
data
in
medical
diagnosis.
The
Quick
Medical
Reference
diagnostic
program
was
used
to
analyze
86
NEJM
CPC
cases
in
three
forms:
intact
cases;
cases
containing
only
history,
physical,
and
admission
type
laboratory
test
results;
and
cases
containing
no
laboratory
test
results.
In
64%
of
the
cases
there
was
no
significant
difference
in
the
performance
of
the
program
using
the
intact
version
of
the
case
versus
using
the
other
two
versions.
Introduction
The
volume
of
medical
laboratory
testing
has
risen
dramatically
in
recent
years.
Possible
explanations
include
proliferation
in
the
number
of
tests
available
due
to
technological
advances,
the
ease
and
efficiency
of
ordering
tests
in
a
"shotgun'
manner,
unquestioned
reimbursement
for
testing
and,
in
part,
concern
over
legal
liability.
The
trend
toward
ordering
more
tests
is
generally
viewed
as
a
problem
rather
than
as
a
necessary
consequence
of
medical
progress.
Efforts
have
been
made
to
address
this
problem
through
identification
of
unnecessary
tests[1],
publication
of
consensus
position
papers
by
professional
organizations,
critical
examination
of
the
indications
for
specific
tests[2],
and
an
attempt
on
the
part
of
third
party
payers
to
disallow
costs
for
tests
or
procedures
which
are
not
indicated.
Other
efforts
have
been
directed
towards
making
better
use
of
the
information
contained
in
the
medical
history
and
physical
examination[3].
An
example
is
the
demonstration
of
the
improved
ability
of
physicians
to
accurately
estimate
the
likelihood
of
coronary
artery
disease
on
the
basis
of
age,
sex,
and
history
of
chest
pain,
when
they
are
provided
with
the
predictive
value
of
the
findings
for
the
disease[4].
It
is
interesting
to
consider
clinicopath-
ological
conference
(CPC)
teaching
cases
in
light
of
attempts
to
more
fully
utilize
the
information
contained
in
the
medical
history.
In
one
sense,
the
CPC
has
evolved
as
a
response
to
the
problem
of
teaching
physicians
how
to
better
utilize
available
information.
The
editors
of
a
CPC
case
usually
present
the
case
at
a
point
at
which
the
diagnosis
can
be
made
only
by
full
use
of
the
information
at
hand.
However,
the
editors
must
also
choose
a
point
that
would
challenge
a
human
expert.
Since
the
ability
of
humans
to
process
information
of
this
type
is
limited[5],
we
hypothesized
that
it
might
be
possible
for
a
computerized
diagnostic
decision
support
system
diagnostic
system,
such
as
the
Quick
Medical
Reference
(QMR)
program,
to
perform
well
with
less
clinical
information.
We
decided
to
determine
how
often
information
from
the
medical
history
and
physical
examination
alone
was
sufficient
for
accurate
diagnosis.
We
also
examined
case
analyses
using
only
the
history,
physical
exam,
and
"admission"
type
laboratory
data.
Methods
Massachusetts
General
Hospital
CPC
cases
published
in
The
New
England
Journal
of
Medicine
(NEJM)
from
1983
to
1988
were
used
as
the
source
of
study
cases.
Over
the
past
decade,
Dr.
Jack
Myers
has
extracted
the
historical
features,
physical
examination
findings,
and
laboratory
values
from
these
cases
for
entry
into
the
INTERNIST-I
and
the
QMR
programs.
Case
descriptions
from
a
139
0195-4210/89/0000/0139$01.00
©
1989
SCAMC,
Inc.
consecutive
series
were
chosen
for
study
purposes.
Cases
were
excluded
from
analysis
if
the
correct
diagnosis
was
not
included
in
the
QMR
knowledge
base.
Eighty-six
cases
formed
the
study
set.
The
analysis
was
performed
using
the
case
analysis
mode
of
QMR.
When
case
specific
information
is
entered
into
QMR,
the
case
analysis
mode
uses
this
information
to
generate
a
ranked
list
of
diagnoses
in
order
of
heuristically
determined
likelihood.
QMR
orders
diagnoses
based
on
a
scoring
function
which
is
similar
to
that
used
by
INTERNIST-I
(QMR
and
INTERNIST-I
are
well
described
elsewhere
[6,7,8]).
The
list
includes
all
diagnoses
with
scores
within.
100
points
of
the
score
of
the
top
diagnosis,
unless
the
score
of
the
top
diagnosis
is
very
low.
In
this
case,
the
range
of
scores
included
is
adjusted
downward.
Each
case
was
analyzed
in
three
ways.
The
initial
analysis
utilized
all
history,
physical
and
laboratory
findings
available
to
the
CPC
discussant
We
termed
this
unedited
version
of
the
CPC
case
"intact".
Two
additional
analyses
were
performed
using
subsets
of
the
"intact"
case
description.
The
second
analysis,
termed
"admission",
was
performed
using
history
and
physical
findings,
and
the
results
of
routine
"admission"
laboratory
tests.
"Admission"
laboratory
tests
included
results
of
complete
blood
count,
peripheral
blood
smear,
serum
electrolytes,
blood
glucose,
fecal
test
for
occult
blood,
blood
urea
nitrogen,
serum
creatinine,
urinalysis,
chest
radiograph,
platelet
count,
and
electrocardiogram.
Any
laboratory
test
which
was
not
an
"admission"
lab
was
termed
a
"special"
laboratory
test.
The
third
and
final
analysis
was
run
using
only
findings
from
the
medical
history
and
physical
examination.
This
version
of
the
case
was
termed
"H&P".
Since
QMR
treats
many
high
level
pathophysiologic
states
or
syndromes
as
diseases,
it
was
possible
for
a
state,
such
as
exudative
pleural
effusion,
to
lead
the
list
of
diagnostic
possibilities.
Because
NEJM
CPC
diagnoses
usually
describe
a
precise
diagnostic
etiology,
we
required
in
our
protocol
that
QMR
also
be
run
until
it
reached
an
etiologica!
diagnosis.
Therefore,
if
a
state
or
syndrome
was
listed
as
the
leading
diagnostic
consideration
by
the
program,
we
asserted
that
state
to
be
present
and
removed
specific
findings.
A
finding
was
removed
if
the
weights
associated
with
the
finding
and
the
state
exceeded
a
fixed,
predetermined
threshold.
The
ranked
differential
diagnosis
list
generated
by
QMR
for
each
of
the
three
analyses
was
then
compared
to
the
"correct"
diagnosis.
We
defined
the
correct
diagnosis
to
be
the
diagnosis
given
in
the
"Anatomical
Diagnosis"
section
of
the
CPC
report
if
the
anatomical
diagnosis
was
single.
If
there
was
more
than
one
diagnosis
for
the
case,
then
the
primary
diagnosis
was
defined
to
be
the
first
diagnosis
listed
by
the
pathologists,
if
the
other
diagnoses
were
not
related
causally.
If
causally
related
diagnosis
were
on
the
list,
then
the
primary
diagnosis
was
defined
to
be
the
causative
diagnosis.
The
position
of
the
correct
diagnosis
in
QMR's
ranked
list
of
diagnostic
possibilities
was
recorded
for
each
of
the
three
analyses
("intact",
"admission",
and
"H&P").
Our
analysis
was
limited
to
the
primary
diagnosis
because
we
did
not
cycle
the
program
to
make
secondary
diagnoses.
For
puposes
of
analysis
we
determined
the
frequency
with
which
the
correct
diagnosis
was
ranked
first,
ranked
within
the
top
three
diagnoses,
ranked
within
the
top
five
diagnoses,
and
within
the
top
ten
diagnoses
on
the
QMR
generated
diagnosis
list.
Tests
of
equality
of
two
regression
lines
were
used
to
compare
the
proportions
of
correct
diagnoses
for
each
mode
of
case
analysis[9].
An
extension
of
the
analysis
was
performed
to
determine
the
proportion
of
cases
in
which
the
addition
of
laboratory
data
actually
made
a
clinically
significant
difference
in
the
program's
ability
to
determine
the
correct
diagnosis.
For
these
purposes
we
created
broader
categories
by
merging
some
of
the
initial
categories.
We
considered
the
rank
of
the
correct
diagnosis
within
four
categories:
a)
the
correct
diagnosis
was
in
position
1-3
on
QMR's
list,
b)
the
correct
diagnosis
was
in
position
4-10
on
QMR's
list,
c)
the
correct
diagnosis
was
in
a
position
greater
than
10
on
QMR's
list,
and
d)
the
correct
diagnosis
was
not
"on the
list"
at
all.
These
categories
were
based
on
our
experience
using
QMR
in
clinical
practice.
140
The
performance
of
the
program
was
assessed
in
the
following
manner
using
each
of
the
three
described
formats
of
cases.
A
significant
change
in
category
was
defined
as
occurring
when
the
position
of
the
"correct"
diagnosis
changed
to
a
lower
category
as
defined
above
(e.g.
from
category
'b"
to
category
"d").
When
the
deletion
of
laboratory
information
from
a
case
record
did
not
result
in
a
change
in
category,
we
considered
this
to
be
an
insignificant
change.
We
considered
any
improvement
in
category
resulting
from
deletion
of
laboratory
findings
to
be
insignificant,
since
our
hypothesis
was
that
such
a
removal
would
affect
performance
adversely.
Resu
Its
A
total
of
86
NEJM
CPC
cases
was
analyzed.
A
single
diagnosis
was
present
in
47/86
(55%)
of
the
cases,
28/86
(33%)
had
two
diagnoses,
and
13/86
(13%)
had
three
or
more
diagnoses.
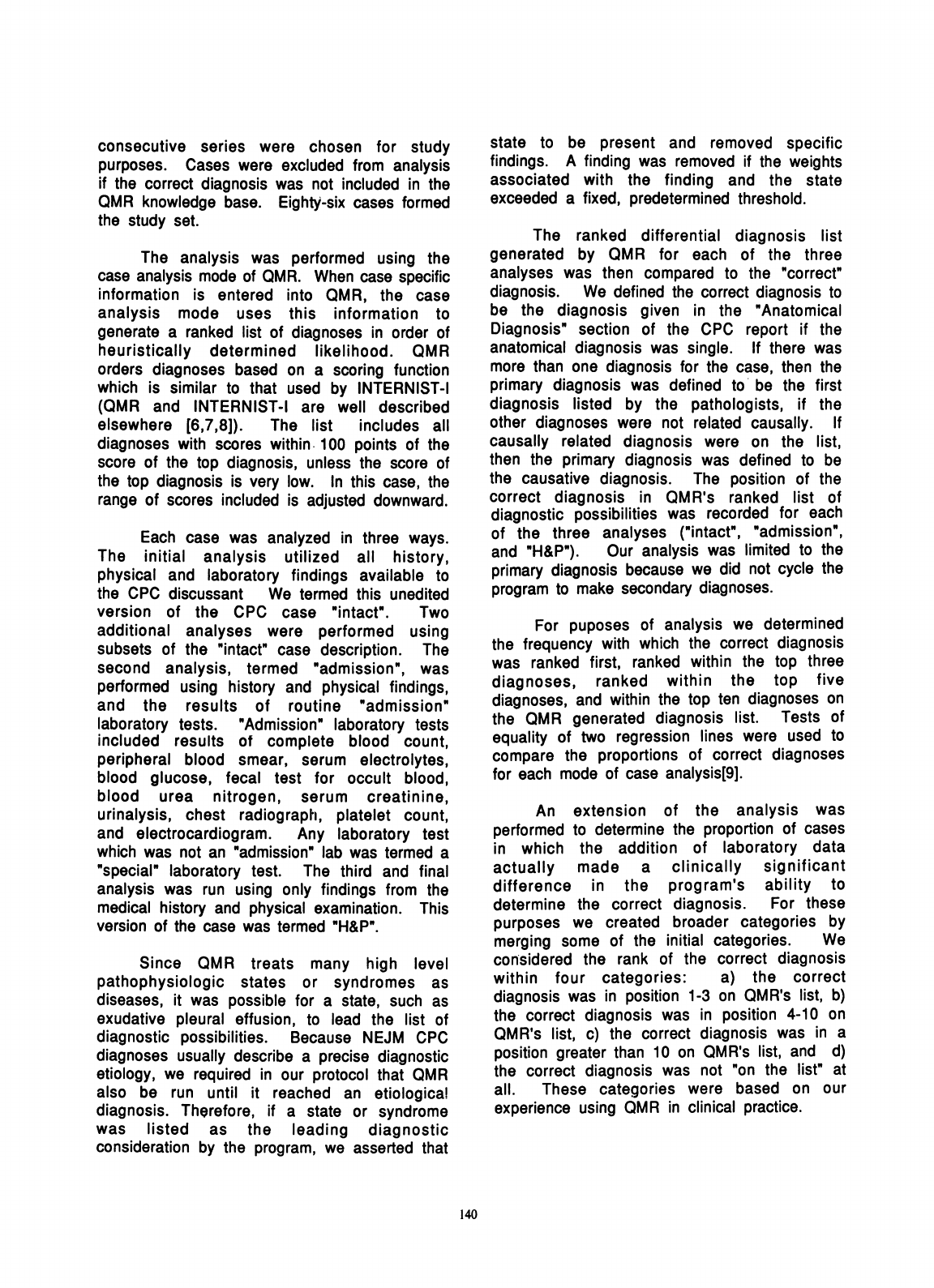
The
average
numbers
of
total
findings,
total
laboratory
findings,
"admission"
laboratory
findings,
and
"special"
laboratory
findings
are
shown
in
Table
1.
The
average
number
of
findings
used
to
represent
a
NEJM
CPC
case
in
the
QMR
vocabulary
was
76.
Of
these
49%
were
laboratory
findings
and
51%
were
findings
from
the
medical
history
and
physical
examination.
Of
the
laboratory
findings,
13/37
(35%)
were
in
the
"admission"
category
and
24/37
(65%)
were
"special"
laboratory
tests.
On
the
average,
24
laboratory
findings
were
eliminated
from
the
intact
case
to
obtain
the
"admission"
case
(Table
1).
TABLE
1.
Description
of
Findings
for
CPC
Cases
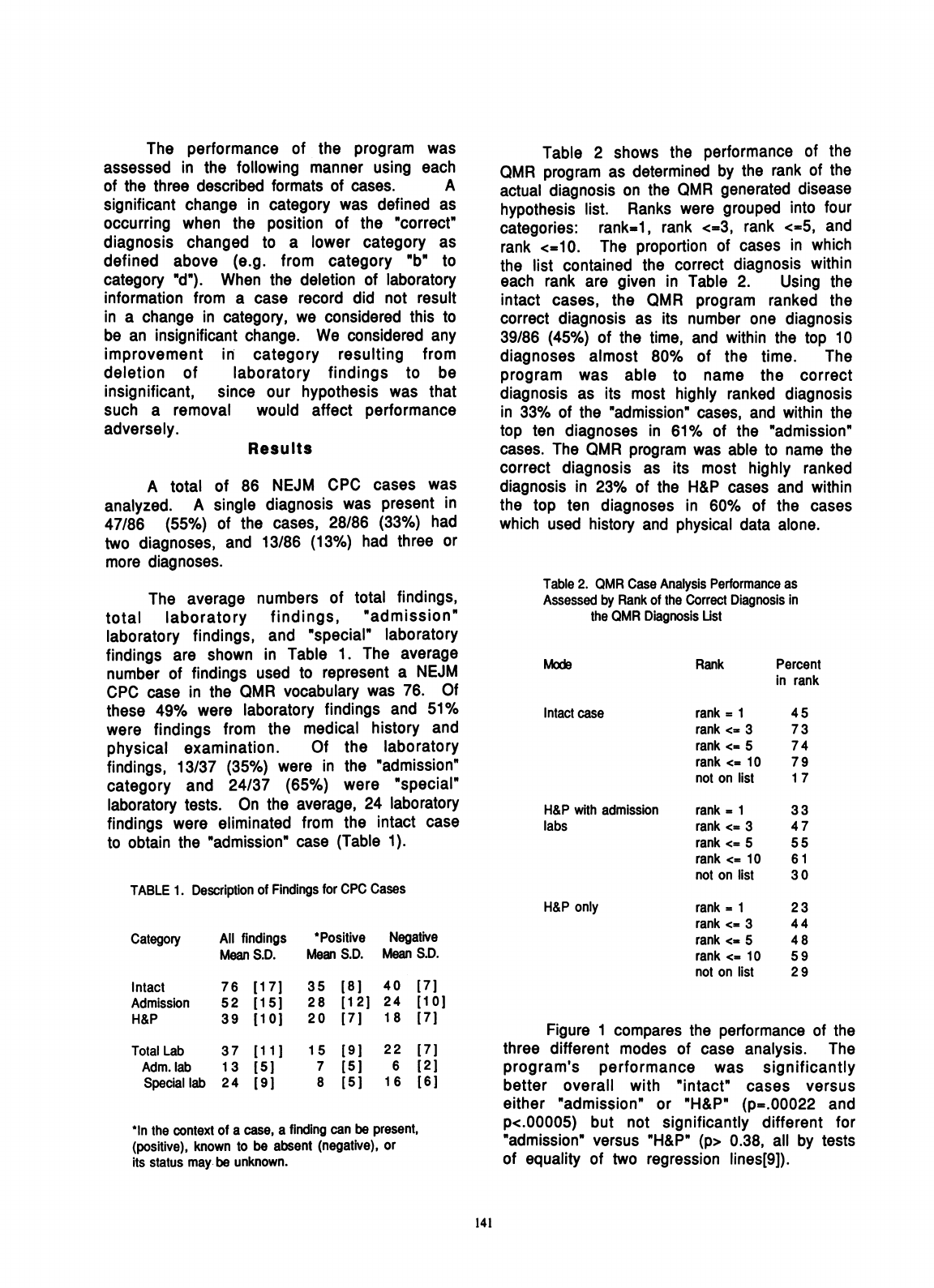
Table
2
shows
the
performance
of
the
QMR
program
as
determined
by
the
rank
of
the
actual
diagnosis
on
the
QMR
generated
disease
hypothesis
list.
Ranks
were
grouped
into
four
categories:
rank=i,
rank
<=3,
rank
<=5,
and
rank
<=10.
The
proportion
of
cases
in
which
the
list
contained
the
correct
diagnosis
within
each
rank
are
given
in
Table
2.
Using
the
intact
cases,
the
QMR
program
ranked
the
correct
diagnosis
as
its
number
one
diagnosis
39/86
(45%)
of
the
time,
and
within
the
top
10
diagnoses
almost
80%
of
the
time.
The
program
was
able
to
name
the
correct
diagnosis
as
its
most
highly
ranked
diagnosis
in
33%
of
the
"admission"
cases,
and
within
the
top
ten
diagnoses
in
61%
of
the
"admission"
cases.
The
QMR
program
was
able
to
name
the
correct
diagnosis
as
its
most
highly
ranked
diagnosis
in
23%
of
the
H&P
cases
and
within
the
top
ten
diagnoses
in
60%
of
the
cases
which
used
history
and
physical
data
alone.
Table
2.
QMR
Case
Analysis
Performance
as
Assessed
by
Rank
of
the
Correct
Diagnosis
in
the
QMR
Diagnosis
Ust
Mods
Rank
Intact
case
H&P
with
admission
labs
H&P
only
Category
All
findings
*Positive
Negative
Mean
S.D.
Mean
S.D.
Mean
S.D.
Intact
Admission
H&P
Total
Lab
Adm.
lab
Special
lab
76
52
39
37
1
3
24
[1
7
[1
5]
[10
]
[
11]
[5]
[91
35
28
20
1
5
7
8
[81
40
[7]
[121
24
[10]
[7]
18
[7]
[91
[5]
[51
22
[7]
6
[21
1
6
[
6]
*In
the
context
of
a
case,
a
finding
can
be
present,
(positive),
known
to
be
absent
(negative),
or
its
status
may
be
unknown.
rank
=
1
rank
<=
3
rank
<.
5
rank
<.
10
not
on
list
rank
=
1
rank
<=
3
rank
<=
5
rank
<=
10
not
on
list
rank
=
1
rank
<=
3
rank
<=
5
rank
<=
10
not
on
list
Percent
in
rank
45
73
74
79
1
7
33
47
55
6
1
30
23
44
48
59
29
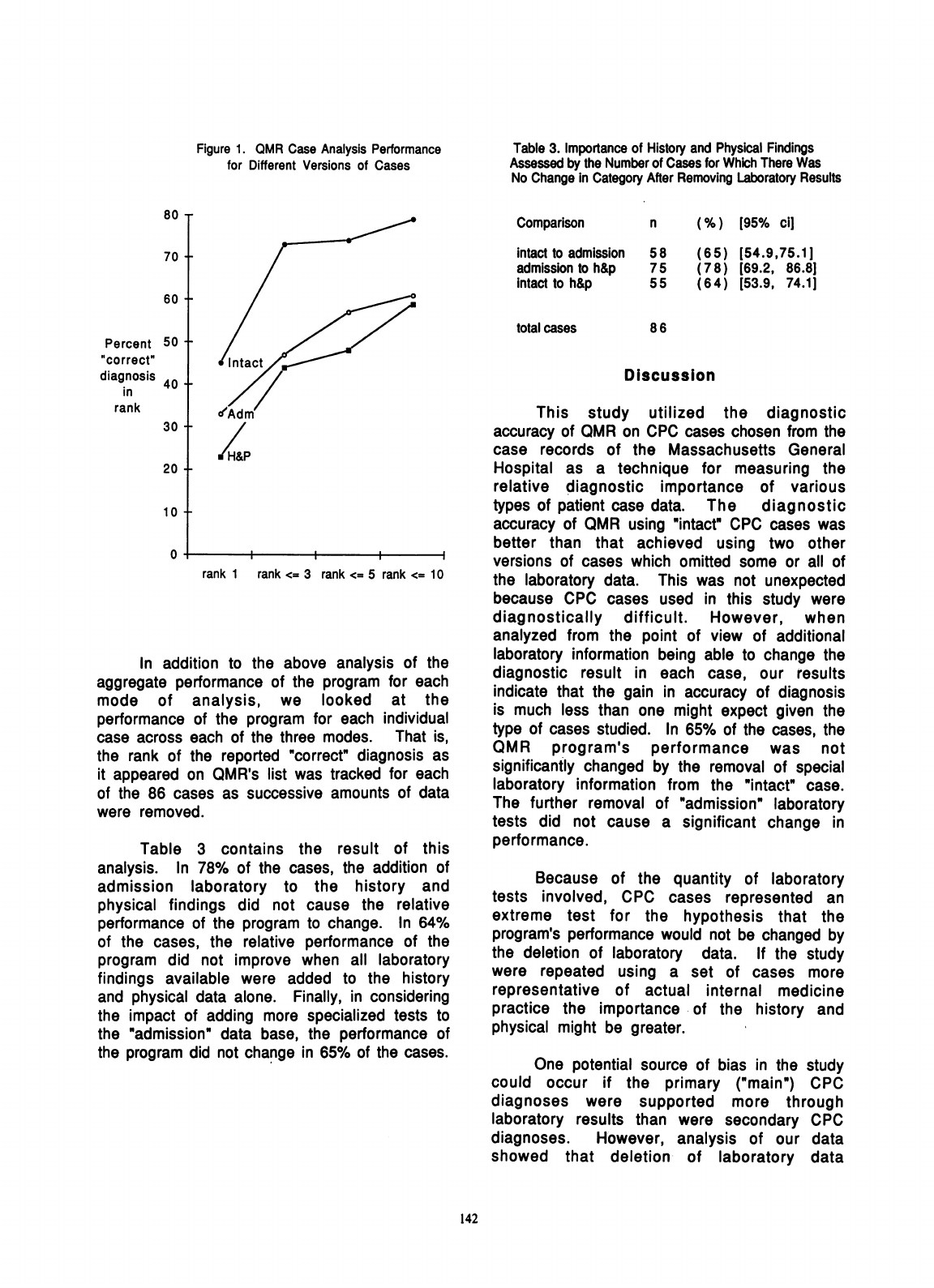
Figure
1
compares
the
performance
of
the
three
different
modes
of
case
analysis.
The
program's
performance
was
significantly
better
overall
with
"intact"
cases
versus
either
"admission"
or
"H&P"
(p=.00022
and
p<.00005)
but
not
significantly
different
for
"admission"
versus
"H&P"
(p>
0.38,
all
by
tests
of
equality
of
two
regression
lines[9]).
141
Figure
1.
QMR
Case
Analysis
Performance
for
Different
Versions
of
Cases
Table
3.
Importance
of
History
and
Physical
Findings
Assessed
by
the
Number
of
Cases
for
Which
There
Was
No
Change
in
Category
After
Removing
Laboratory
Results
80
T
70
+
60
+
Percent
50
f
ofcorrect"
diagnosis
40
in
rank
30
+
20
-
10
-
0
7
Intact
cIAdm
rank
1
rank
<=
3
rank
<=
5
In
addition
to
the
above
analy
aggregate
performance
of
the
progran
mode
of
analysis,
we
looked
performance
of
the
program
for
each
case
across
each
of
the
three
modes.
the
rank
of
the
reported
"correct"
die
it
appeared
on
QMR's
list
was
tracke4
of
the
86
cases
as
successive
amour
were
removed.
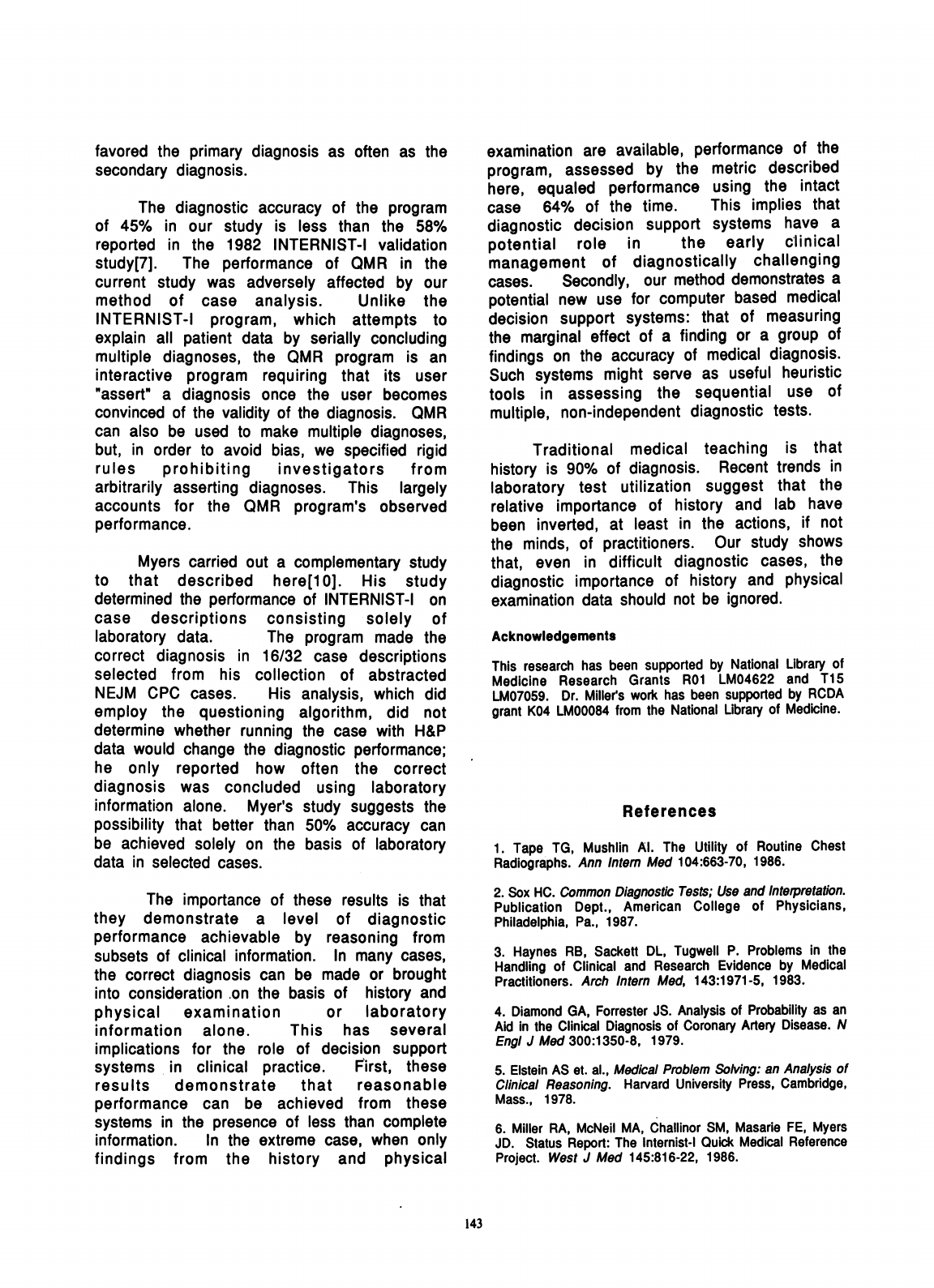
Table
3
contains
the
resul
analysis.
In
78%
of
the
cases,
the
admission
laboratory
to
the
his
physical
findings
did
not
cause
th
performance
of
the
program
to
change
of
the
cases,
the
relative
performan
program
did
not
improve
when
all
findings
available
were
added
to
tl
and
physical
data
alone.
Finally,
in
c
the
impact
of
adding
more
specialize
the
"admission"
data
base,
the
perfo
the
program
did
not
change
in
65%
of
Comparison
intact
to
admission
admission
to
h&p
intact
to
h&p
total
cases
c
n
(%)
[95%
ci]
58
75
55
(65)
[54.9,75.1]
(7
8)
[69.2,
86.8]
(64)
[53.9,
74.1]
86
Discussion
This
study
utilized
the
diagnostic
accuracy
of
QMR
on
CPC
cases
chosen
from
the
case
records
of
the
Massachusetts
General
Hospital
as
a
technique
for
measuring
the
relative
diagnostic
importance
of
various
types
of
patient
case
data.
The
diagnostic
accuracy
of
QMR
using
"intact"
CPC
cases
was
better
than
that
achieved
using
two
other
versions
of
cases
which
omitted
some
or
all
of
;rank
<=
10
the
laboratory
data.
This
was
not
unexpected
because
CPC
cases
used
in
this
study
were
diagnostically
difficult.
However,
when
analyzed
from
the
point
of
view
of
additional
,sis
of
the
laboratory
information
being
able
to
change
the
n
for
each
diagnostic
result
in
each
case,
our
results
at
orhea
indicate
that
the
gain
in
accuracy
of
diagnosis
individual
is
much
less
than
one
might
expect
given
the
That
is
type
of
cases
studied.
In
65%
of
the
cases,
the
ignosis
as
QMR
program's
performance
was
not
d
for
each
significantly
changed
by
the
removal
of
special
its
of
data
laboratory
information
from
the
"intact"
case.
The
further
removal
of
"admission"
laboratory
tests
did
not
cause
a
significant
change
in
t
of
this
performance.
addition
of
Because
of
the
quantity
of
laboratory
-tory
and
le
rellative
tests
involved,
CPC
cases
represented
an
a.
In
64%
extreme
test
for
the
hypothesis
that
the
ace
of
the
program's
performance
would
not
be
changed
by
laboratory
the
deletion
of
laboratory
data.
If
the
study
he
history
were
repeated
using
a
set
of
cases
more
onsidering
representative
of
actual
internal
medicine
d
tests
to
practice
the
importance
of
the
history
and
rmance
of
physical
might
be
greater.
the
cases.
One
potential
source
of
bias
in
the
study
could
occur
if
the
primary
("main")
CPC
diagnoses
were
supported
more
through
laboratory
results
than
were
secondary
CPC
diagnoses.
However,
analysis
of
our
data
showed
that
deletion
of
laboratory
data
142
favored
the
primary
diagnosis
as
often
as
the
secondary
diagnosis.
The
diagnostic
accuracy
of
the
program
of
45%
in
our
study
is
less
than
the
58%
reported
in
the
1982
INTERNIST-I
validation
study[7].
The
performance
of
QMR
in
the
current
study
was
adversely
affected
by
our
method
of
case
analysis.
Unlike
the
INTERNIST-I
program,
which
attempts
to
explain
all
patient
data
by
serially
concluding
multiple
diagnoses,
the
QMR
program
is
an
interactive
program
requiring
that
its
user
"assert"
a
diagnosis
once
the
user
becomes
convinced
of
the
validity
of
the
diagnosis.
QMR
can
also
be
used
to
make
multiple
diagnoses,
but,
in
order
to
avoid
bias,
we
specified
rigid
rules
prohibiting
investigators
from
arbitrarily
asserting
diagnoses.
This
largely
accounts
for
the
QMR
program's
observed
performance.
Myers
carried
out
a
complementary
study
to
that
described
here[1
0].
His
study
determined
the
performance
of
INTERNIST-I
on
case
descriptions
consisting
solely
of
laboratory
data.
The
program
made
the
correct
diagnosis
in
16/32
case
descriptions
selected
from
his
collection
of
abstracted
NEJM
CPC
cases.
His
analysis,
which
did
employ
the
questioning
algorithm,
did
not
determine
whether
running
the
case
with
H&P
data
would
change
the
diagnostic
performance;
he
only
reported
how
often
the
correct
diagnosis
was
concluded
using
laboratory
information
alone.
Myer's
study
suggests
the
possibility
that
better
than
50%
accuracy
can
be
achieved
solely
on
the
basis
of
laboratory
data
in
selected
cases.
The
importance
of
these
results
is
that
they
demonstrate
a
level
of
diagnostic
performance
achievable
by
reasoning
from
subsets
of
clinical
information.
In
many
cases,
the
correct
diagnosis
can
be
made
or
brought
into
consideration
on
the
basis
of
history
and
physical
examination
or
laboratory
information
alone.
This
has
several
implications
for
the
role
of
decision
support
systems
in
clinical
practice.
First,
these
results
demonstrate
that
reasonable
performance
can
be
achieved
from
these
systems
in
the
presence
of
less
than
complete
information.
In
the
extreme
case,
when
only
findings
from
the
history
and
physical
examination
are
available,
performance
of
the
program,
assessed
by
the
metric
described
here,
equaled
performance
using
the
intact
case
64%
of
the
time.
This
implies
that
diagnostic
decision
support
systems
have
a
potential
role
in
the
early
clinical
management
of
diagnostically
challenging
cases.
Secondly,
our
method
demonstrates
a
potential
new
use
for
computer
based
medical
decision
support
systems:
that
of
measuring
the
marginal
effect
of
a
finding
or
a
group
of
findings
on
the
accuracy
of
medical
diagnosis.
Such
systems
might
serve
as
useful
heuristic
tools
in
assessing
the
sequential
use
of
multiple,
non-independent
diagnostic
tests.
Traditional
medical
teaching
is
that
history
is
90%
of
diagnosis.
Recent
trends
in
laboratory
test
utilization
suggest
that
the
relative
importance
of
history
and
lab
have
been
inverted,
at
least
in
the
actions,
if
not
the
minds,
of
practitioners.
Our
study
shows
that,
even
in
difficult
diagnostic
cases,
the
diagnostic
importance
of
history
and
physical
examination
data
should
not
be
ignored.
Acknowledgements
This
research
has
been
supported
by
National
Library
of
Medicine
Research
Grants
ROI
LM04622
and
T15
LM07059.
Dr.
Millers
work
has
been
supported
by
RCDA
grant
K04
LM00084
from
the
National
Library
of
Medicine.
References
1.
Tape
TG,
Mushlin
Al.
The
Utility
of
Routine
Chest
Radiographs.
Ann
Intem
Med
104:663-70,
1986.
2.
Sox
HC.
Common
Diagnostic
Tests;
Use
and
Interpretation.
Publication
Dept.,
American
College
of
Physicians,
Philadelphia,
Pa.,
1987.
3.
Haynes
RB,
Sackett
DL,
Tugwell
P.
Problems
in
the
Handling
of
Clinical
and
Research
Evidence
by
Medical
Practitioners.
Arch
Intem
Med,
143:1971-5,
1983.
4.
Diamond
GA,
Forrester
JS.
Analysis
of
Probability
as
an
Aid
in
the
Clinical
Diagnosis
of
Coronary
Artery
Disease.
N
Engi
J
Med
300:1350-8,
1979.
5.
Elstein
AS
et.
al.,
Medical
Problem
Solving:
an
Analysis
of
Clinical
Reasoning.
Harvard
University
Press,
Cambridge,
Mass.,
1978.
6.
Miller
RA,
McNeil
MA,
Challinor
SM,
Masarie
FE,
Myers
JD.
Status
Report:
The
Internist-I
Quick
Medical
Reference
Project.
West
J
Med
145:816-22,
1986.
143
7.
Miller
RA,
Pople
HE,
Myers
JD.
INTERNIST-I,
An
Experimental
Computer-based
Diagnostic
Consultant
for
General
Internal
Medicine.
N
Engl
J
Med
307:468-76,
1982.
8
Masarie
FE,
Miller
RA.
INTERNIST-I
to
Quick
Medical
Reference
(QMR):
The
Transition
from
a
Mainframe
to
a
Microcomputer.
Proc.
Ninth
Annual
IEEE/Engineering
in
Medicine
and
Biology
Society,
IEEE
Press,
Boston,
Mass.,
1521-2,
1987.
9.
Kleinbaum
DG,
Kupper
LL.
Applied
Regression
Analysis
and
Other
Multivariable
Methods.
Duxbury
Press,
Boston,
Mass.,
1978.
10.
Myers
JD.
The
Computer
as
a
Diagnostic
Consultant,
with
Emphasis
on
Use
of
Laboratory
Data.
Clinical
Chemistry,
32(9):1714-18,
1986.
144
