
Technical Volume 2:
Cybersecurity Practices for
Medium and Large Healthcare
Organizations
2023 Edition

iTechnical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table of Contents
Introduction 1
Cybersecurity Practices at Medium-Sized Healthcare Organizations 2
IT Assets Used by Medium-Sized Organizaons ................................................................................................................................... 3
Cybersecurity Pracces ........................................................................................................................................................................................... 4
Cybersecurity Practices at Large Healthcare Organizations 5
IT Assets Used by Large Organizaons .........................................................................................................................................................6
Document Guide: Cybersecurity Practices 8
Cybersecurity Practice #1: Email Protection Systems 13
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................13
1.M.A: Basic Email Protection Controls ................................................................................................................................................. 13
1.M.B: Multi-Factor Authentication for Email Access..................................................................................................................16
1.M.C: Email Encryption
....................................................................................................................................................................................16
1.M.D: Workforce Education .........................................................................................................................................................................17
Sub-Pracces for Large Organizaons .......................................................................................................................................................20
1.L.A: Advanced and Next-Generation Tooling ................................................................................................................................. 20
1.L.B: Digital Signatures .................................................................................................................................................................................... 21
1.L.C: Analytics-Driven Education .............................................................................................................................................................22
Key Migated Threats ............................................................................................................................................................................................ 22
Suggested Metrics ....................................................................................................................................................................................................22
Cybersecurity Practice #2: Endpoint Protection Systems 24
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................24
2.M.A: Basic Endpoint Protection Controls.........................................................................................................................................24
2.M.B: Mobile Device and Mobile Application Management
.................................................................................................. 27
Sub-Pracces for Large Organizaons .......................................................................................................................................................28
2.L.A: Automate the Provisioning of Endpoints ................................................................................................................................28
2.L.B: Host-Based Intrusion Detection and Prevention Systems ......................................................................................... 29
2.L.C: Endpoint Detection and Response .............................................................................................................................................. 29
2.L.D: Application Allowlisting .....................................................................................................................................................................31
2.L.E: Micro-Segmentation/Virtualization Strategies ..................................................................................................................33
Key Migated Threats ............................................................................................................................................................................................ 33
Suggested Metrics ....................................................................................................................................................................................................34
Cybersecurity Practice #3: Identity and Access Management 35
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................35
3.M.A: Identity ......................................................................................................................................................................................................... 35
3.M.B: Provisioning, Transfers and Deprovisioning Procedures ........................................................................................... 37
3.M.C: Authentication ........................................................................................................................................................................................38
3.M.D: Multifactor Authentication............................................................................................................................................................41
Sub-Pracces for Large Organizaons
.......................................................................................................................................................42
3.L.A: Federated Identity Management .................................................................................................................................................42
3.L.B: Authorization ............................................................................................................................................................................................. 43
3.L.C: Access Governance ................................................................................................................................................................................44

iiTechnical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
3.L.D: Single Sign-On (SSO) .............................................................................................................................................................................45
Key Migated Threats ............................................................................................................................................................................................ 45
Suggested Metrics ....................................................................................................................................................................................................45
Cybersecurity Practice #4: Data Protection and Loss Prevention 46
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................47
4.M.A: Classication of Data..........................................................................................................................................................................47
4.M.B: Data Use Procedures
..........................................................................................................................................................................48
4.M.C: Data Security ............................................................................................................................................................................................49
4.M.D: Backup Strategies ................................................................................................................................................................................. 50
4.M.E: Data Loss Prevention (DLP)............................................................................................................................................................52
Sub-Pracces for Large Organizaons
.......................................................................................................................................................54
4.L.A: Advanced Data Loss Prevention ................................................................................................................................................... 54
4.L.B: Mapping Data Flows .............................................................................................................................................................................55
Key Migated Threats ............................................................................................................................................................................................ 56
Suggested Metrics ....................................................................................................................................................................................................57
Cybersecurity Practice #5: IT Asset Management 58
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................58
5.M.A: Inventory of Endpoints and Servers ......................................................................................................................................... 58
5.M.B: Procurement.............................................................................................................................................................................................60
5.M.C: Secure Storage for Inactive Devices.........................................................................................................................................60
5.M.D: Decommissioning Assets
.................................................................................................................................................................61
Sub-Pracces for Large Organizaons .......................................................................................................................................................61
5.L.A: Automated Discovery and Maintenance ................................................................................................................................61
5.L.B: Integration with Network Access Control .............................................................................................................................62
Key Migated Threats ............................................................................................................................................................................................ 62
Suggested Metrics ....................................................................................................................................................................................................62
Cybersecurity Practice #6: Network Management 63
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................63
6.M.A: Network Proles and Firewalls ...................................................................................................................................................63
6.M.B: Network Segmentation .....................................................................................................................................................................64
6.M.C: Intrusion Prevention Systems ......................................................................................................................................................66
6.M.D: Web Proxy Protection ....................................................................................................................................................................... 67
6.M.E: Physical Security of Network Devices ....................................................................................................................................68
Sub-Pracces for Large Organizaons .......................................................................................................................................................68
6.L.A: Additional Network Segmentation ............................................................................................................................................. 68
6.L.B: Network Analytics and Blocking ...................................................................................................................................................69
6.L.C: Network Access Control (NAC) ....................................................................................................................................................70
Key Migated Threats ............................................................................................................................................................................................ 71
Suggested Metrics ....................................................................................................................................................................................................71
Cybersecurity Practice #7: Vulnerability Management 72
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................72
7.M.A: Host/Server-Based Scanning ........................................................................................................................................................ 72
7.M.B: Web Application Scanning ..............................................................................................................................................................73
7.M.C: System Placement and Data Classication .........................................................................................................................73
7.M.D: Patch Management, Conguration Management ..........................................................................................................74

iiiTechnical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
7.M.E: Change Management ..........................................................................................................................................................................75
Sub-Pracces for Large Organizaons .......................................................................................................................................................76
7.L.A: Penetration Testing................................................................................................................................................................................76
7.L.B: Vulnerability Remediation Planning
...........................................................................................................................................78
7.L.C: Attack Simulation ....................................................................................................................................................................................79
Key Migated Threats ............................................................................................................................................................................................ 81
Suggested Metrics ....................................................................................................................................................................................................81
Cybersecurity Practice #8: Security Operations Center and Incident Response 82
Sub-Pracces for Medium-Sized Organizaons .................................................................................................................................82
8.M.A: Security Operations Center (SOC)............................................................................................................................................82
8.M.B: Incident Response
................................................................................................................................................................................87
8.M.C: Information Sharing and ISACs/ISAOs ................................................................................................................................... 92
Sub-Pracces for Large Organizaons .......................................................................................................................................................93
8.L.A: Advanced Security Operations Center ....................................................................................................................................93
8.L.B: Advanced Information Sharing ...................................................................................................................................................... 95
8.L.C: Incident Response Orchestration ................................................................................................................................................95
8.L.D: Baseline Network Trafc ...................................................................................................................................................................96
8.L.E: User Behavior Analytics ......................................................................................................................................................................97
8.L.F: Deception Technologies ......................................................................................................................................................................98
Key Migated Threats ............................................................................................................................................................................................ 99
Suggested Metrics ....................................................................................................................................................................................................99
Cybersecurity Practice #9: Network Connected Medical Devices 100
Sub-Pracces for Medium-Sized Organizaons ..............................................................................................................................105
9.M.A: Asset Management ...........................................................................................................................................................................105
9.M.B: Endpoint Protections .......................................................................................................................................................................107
9.M.C: Identity and Access Management ...........................................................................................................................................108
9.M.D: Network Management ................................................................................................................................................................... 110
9.M.E: Vulnerability Management ..........................................................................................................................................................111
9.M.F: Contacting the FDA ........................................................................................................................................................................... 115
Sub-Pracces for Large Organizaons .................................................................................................................................................... 116
9.L.A: Security Operations and Incident Response .....................................................................................................................116
9.L.B: Procurement and Security Evaluations.................................................................................................................................120
Key Migated Threats
.........................................................................................................................................................................................122
Suggested Metrics .................................................................................................................................................................................................123
Cybersecurity Practice #10: Cybersecurity Oversight and Governance 124
Sub-Pracces for Medium-Sized Organizaons ..............................................................................................................................124
10.M.A: Policies ...................................................................................................................................................................................................124
10.M.B: Cybersecurity Risk Assessment and Management ..................................................................................................126
10.M.C: Security Awareness and Training .........................................................................................................................................128
Sub-Pracces for Large-Sized Organizaons .....................................................................................................................................129
10.L.A: Cyber Insurance ................................................................................................................................................................................. 129
Key Migated Threats .........................................................................................................................................................................................131
Suggested Metrics .................................................................................................................................................................................................131
Appendix A: Acronyms and Abbreviations 132
Appendix B: References 136

ivTechnical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
List of Tables
Table 1. Five Prevailing Cybersecurity Threats to Healthcare Organizaons ...................................................................8
Table 2. Email Protecon Controls ................................................................................................................................................................ 14
Table 3. Basic Endpoint Controls to Migate Endpoint Risk ...................................................................................................... 24
Table 4. Example of a Data Classicaon Schema .............................................................................................................................49
Table 5. Suggested Procedures for Data Disclosure ......................................................................................................................... 50
Table 6. Security Methods to Protect Data .............................................................................................................................................50
Table 7. Data Channels for Enforcing Data Policies .......................................................................................................................... 54
Table 8. Expanding DLP to Other Data Channels ...............................................................................................................................55
Table 9. Recommended Timeframes for Migang IT Vulnerabilies .................................................................................76
Table 10. Factors for Consideraon in Penetraon Test Planning .........................................................................................78
Table 11. Example Incident Response Plays for IR Playbooks ..................................................................................................85
Table 12. Roles and Responsibilies for an Organizaonal CIRT ............................................................................................ 89
Table 13. ADS Use Cases ..................................................................................................................................................................................114
Table 14. Timeframes for Resolving Medical Device Vulnerabilies .................................................................................115
Table 15. Incident Response Plays for Aacks Against Medical Devices ....................................................................... 120
Table 16. Example Cybersecurity Policies for Consideraon ..................................................................................................126
Table 17. Acronyms and Abbreviaons...................................................................................................................................................133

1Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Introducon
This volume will help answer the question, “How do I mitigate the ve threats outlined in the
Main Document?”
Technical Volume 2 outlines healthcare cybersecurity best practices for medium-sized and large
healthcare organizations. Medium-sized and large organizations generally have dedicated information
technology (IT) departments, and very likely have dedicated cybersecurity staff. Organizational personnel
typically have an awareness of the cybersecurity threats faced to patients and their organization.
This volume is for the technical practitioner and contains technical details for implementing cybersecurity
practices. It provides an overview of cybersecurity practices that have been outlined by the industry as
highly effective at mitigating risks to the healthcare industry.
This volume is an index of existing industry practices, with guidance on how to start your journey
implementing these practices. Details and explanations of the cybersecurity practices are included for
additional context where needed.
To determine the size of your organization, please refer to Main Document, Table 1. Examples of medium-
sized organizations are community hospitals, critical access hospitals with more than 50 beds, or larger
medical groups. Examples of larger organizations include large health systems with multiple hospitals,
integrated delivery networks, or clinical groups with multiple geographically dispersed locations.
Please consider these simple instructions when reading this volume:
1. If you are a medium-sized organization, start with the sub-practices with the heading “Sub- Practices
for Medium-Sized Organizations.” Feel free to consider the additional sub-practices as well.
2. If you are a large organization, consider implementing all the sub-practices listed in the document,
including both those under the heading “Sub-Practices for Medium-Sized Organizations” as well as
those labeled “Sub-Practices for Large Organizations.”
2Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracces at Medium-
Sized Healthcare Organizaons
Medium-sized healthcare organizations perform critical functions for the healthcare and public health
(HPH) sector. These organizations include critical access hospitals in rural areas, practice management
organizations that support physician practices, revenue cycle or billing organizations, mid-sized device
manufacturers, and group practices. Medium-sized healthcare organizations generally employ hundreds
of personnel, maintain between hundreds and a few thousand IT assets, and may be primary partners
with and liaisons between small and large healthcare organizations. It is typical for a medium-sized
organization to have several critical systems that are interconnected to enable work activities in support
of its mission.
These organizations tend to have a diverse inventory of assets that support multiple revenue streams.
They also tend to have narrow prot margins, limited resources, and limited exibility to implement
robust cybersecurity practices. For example, it is rare for a medium-sized organization to have its own
dedicated 24x7x365 security operations center (SOC).
Medium-sized organizations typically focus on preventing cybersecurity events and implementing
restrictive security policies with few exceptions permitted. These restrictive policies are often due to
insufcient resources to support more open and exible cybersecurity models, such as those larger
organizations can often afford. Medium-sized organizations usually struggle to obtain cybersecurity
funding that is distinct from their standard IT budgets. The top security professionals in an organization
of this size might often feel overwhelmed by compliance and cybersecurity duties, wear multiple hats, and
experience constraints around execution plans.
Medium-sized organizations operate in complex legal and regulatory environments that include, but are
not limited to, the following:
• The Ofce of the National Coordinator for Health Information Technology (ONC) regulations
prohibiting information blocking and promoting the interoperability of Certied Electronic Health
Information Technology
1
• The Medicare Access and Children’s Health Insurance Program Reauthorization Act of 2015
(MACRA)/Meaningful Use
2
• Multiple enforcement obligations under the Food and Drug Administration (FDA)
3
• The Joint Commission or DNV accreditation processes
4
• The Health Insurance Portability and Accountability Act of 1996 (HIPAA)/Health Information
Technology for Economic and Clinical Health Act (HITECH) requirements
5
1 ONC Cures Act Final Rule, https://www.healthit.gov/curesrule/.
2 “MACRA,” Centers for Medicare and Medicaid Services (CMS), https://www.cms.gov/Medicare/Quality-Initiatives-
Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-
APMs#:~:text=The%20Medicare%20Access%20and%20CHIP,clinicians%20for%20value%20over%20volume.
3 “Cybersecurity,” FDA, https://www.fda.gov/medical-devices/digital-health-center-excellence/cybersecurity.
4 “Learn the Process,” The Joint Commission, https://www.jointcommission.org/accreditation-and-certication/
become-accredited/learn-the-process/.
5 “The HIPAA Privacy Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
“HITECH Act Enforcement Interim Final Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/special-topics/
hitech-act-enforcement-interim-nal-rule/index.html.

Cybersecurity Practices at Medium-Sized Healthcare Organizations
3Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• The Payment Card Industry Data Security Standard (PCI-DSS1)
6
• Substance Abuse and Mental Health Services Administration (SAMHSA) requirements (42 CFR
part 2)
7
• The Gramm-Leach-Bliley Act for nancial processing
8
• The Family Educational Rights and Privacy Act (FERPA) for those institutions participating within
Higher Education
9
• The Genetic Information Nondiscrimination Act (GINA)
10
• The General Data Protection Regulation (GDPR) in the European Union
11
• State laws setting standards for privacy and security such as the California Consumer Privacy
Act (CCPA)
12
Changes to the Stark Law Physician self-referral regulations and the related anti-kickback statute took
effect in January 2021. These protect the donation of cybersecurity technology and services that are
“necessary and used predominantly to implement, maintain, reestablish effective cybersecurity.”
13
IT Assets Used by Medium-Sized Organizations
Medium-sized organizations may have up to a few thousand IT assets. All assets may have cybersecurity
vulnerabilities and are therefore susceptible to cyber threats. There are three important factors
in securing assets: (1) understanding their relationship within your organization’s IT ecosystem; (2)
understanding how the workforce leverages and uses the assets; and (3) understanding the data that are
generated, stored, and processed within those assets.
Not all assets are equally important; some are mission critical and must be fully operational due to patient
safety, while others are less critical, and might even be ofine for days or weeks without harming your
organization’s mission. Some assets are critical for patient care, such as bedside monitors, whereas
others have large repositories of sensitive data that represent signicant risk but are not as critical to
the enterprise’s business. In all cases, your organization uses IT assets for business reasons and should
protect those assets with proper cyber hygiene controls.
Examples of assets found in medium-sized organizations include, but are not limited to, the following:
• Static devices used by the workforce, such as shared workstations and clinical workstations used
strictly for patient care with select mobile devices, such as laptops and smartphones. Due to budget
restrictions, medium-sized organizations may not maintain many mobile devices.
6 “PCI DSS v4.0 Resource Hub,” PCI Security Standards Council, https://www.pcisecuritystandards.org/.
7 “Registration Requirements,” SAMHSA, https://www.samhsa.gov/grants/applying/registration-requirements.
8 “Gramm-Leach-Bliley Act,” FTC, https://www.ftc.gov/business-guidance/privacy-security/gramm-leach-bliley-act.
9 “Family Educational Rights and Privacy Act (FERPA),” US Department of Education, https://www2.ed.gov/policy/gen/
guid/fpco/ferpa/index.html.
10 “Genetic Information,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/special-topics/genetic-information/
index.html.
11 “General Data Protection Regulation: GDPR,” Intersoft Consulting, https://gdpr-info.eu/.
12 “California Consumer Privacy Act (CCPA),” State of California Department of Justice, https://oag.ca.gov/privacy/ccpa.
13 The Stark Law, 42 C.F.R. § 411.357(bb)(1) and the Anti-Kickback Statute, 42 C.F.R. § 1001.952(jj) are the result of the
CMS Final Rule at 85 Fed. Reg. 77,492 (December 2, 2020).

Cybersecurity Practices at Medium-Sized Healthcare Organizations
4Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Internet of things (IoT) devices, such as smart televisions, medical devices, thermometers, printers,
copiers, and security cameras.
• Data that includes sensitive health information stored and processed on devices, servers, applications,
and the cloud. These data include names, medical record numbers, birth dates, Social Security
numbers (SSNs), diagnostic conditions, prescriptions, mental health issues, substance abuse, or
sexually transmitted disease information. Individually identiable health information (IIHI) about a
patient that is created or maintained by a HIPAA covered entity is protected health information (PHI)
and must be safeguarded against unauthorized use or disclosure.
• Assets related to the IT infrastructure, such as rewalls, network switches and routers, Wi-Fi
networks (both corporate and guest), servers supporting IT management systems, and le storage
systems (cloud-based or onsite).
• Applications or information systems that support the business processes. These may include
human resource (HR) or enterprise resource planning (ERP) systems, pathology lab systems, blood
bank systems, medical imaging systems, pharmacy systems, revenue cycle systems, supply chain or
materials management systems, specialized oncology therapy systems, radiation oncology treatment
systems, and data warehouses (e.g., clinical, nancial).
Personal devices, often referred to as “bring your own device” (BYOD), are often not permitted in
medium-sized organizations due to its inability to implement dedicated security controls required to
secure such devices.
Cybersecurity Practices
At a minimum, medium-sized organizations should consider implementing the Sub-Practices for Medium-
Sized Organizations discussed in each cybersecurity practice presented in this volume. However, medium-
sized organizations may additionally adopt the cybersecurity practices used by large organizations.
Organizations should consider adopting any cybersecurity practice determined to be relevant.

5Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracces at Large
Healthcare Organizaons
Large healthcare organizations perform a range of different functions. These organizations may be
integrated with other healthcare delivery organizations, academic medical centers, insurers that provide
healthcare coverage, clearinghouses, pharmaceuticals, or medical device manufacturers. In most cases,
large organizations employ thousands of employees, maintain tens of thousands to hundreds of thousands
of IT assets, and have intricate and complex digital ecosystems. Whereas smaller organizations operate
using only a few critical systems, large organizations can have hundreds or thousands of interconnected
systems with complex functionality.
The missions of large organizations are diverse and varied. They include providing standard general
practice care, providing specialty or subspecialty care for complicated medical cases, conducting
innovative medical research, providing insurance coverage to large populations of patients, supporting the
healthcare delivery ecosystem, and supplying and researching new therapeutic treatments (such as drugs
or medical devices).
Large organizations have missions that are broad in scope, and large volumes of assets may be necessary
to fulll such missions. They often struggle to obtain funding to maintain security programs and control
their assets (potentially resulting in shadow IT, rogue devices, and unmanaged/unpatched devices).
Therefore, it is essential for large organizations to understand how sensitive data ow in and out of
their organization, and to understand the boundaries and segments that determine where one entity’s
responsibilities end, and another’s start.
Large organizations operate in a legal and regulatory environment that is as complicated as their digital
ecosystems. This environment includes, but is not limited to, the following references:
• The Ofce of the National Coordinator for Health Information Technology (ONC) regulations
prohibiting information blocking and promoting the interoperability of Certied Electronic Health
Information Technology
14
• The Medicare Access and Children’s Health Insurance Program Reauthorization Act of 2015
(MACRA)/Meaningful Use
15
• Multiple enforcement obligations under the Food and Drug Administration (FDA)
16
• The Joint Commission or DNV accreditation processes
17
• The Health Insurance Portability and Accountability Act of 1996 (HIPAA)/Health Information
Technology for Economic and Clinical Health Act (HITECH) requirements
18
14 ONC Cures Act Final Rule, https://www.healthit.gov/curesrule/.
15 “MACRA,” Centers for Medicare and Medicaid Services (CMS), https://www.cms.gov/Medicare/Quality-Initiatives-
Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-
APMs#:~:text=The%20Medicare%20Access%20and%20CHIP,clinicians%20for%20value%20over%20volume.
16 “Cybersecurity,” FDA, https://www.fda.gov/medical-devices/digital-health-center-excellence/cybersecurity.
17 “Learn the Process,” The Joint Commission, https://www.jointcommission.org/accreditation-and-certication/
become-accredited/learn-the-process/.
18 “The HIPAA Privacy Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
“HITECH Act Enforcement Interim Final Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/special-topics/
hitech-act-enforcement-interim-nal-rule/index.html.

Cybersecurity Pracces at Large Healthcare Organizaons
6Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• The Payment Card Industry Data Security Standard (PCI-DSS1)
19
• Substance Abuse and Mental Health Services Administration (SAMHSA) requirements (42 CFR
part 2)
20
• The Gramm-Leach-Bliley Act for nancial processing
21
• The Stark Law as it relates to providing services to afliated organizations
22
• The Family Educational Rights and Privacy Act (FERPA) for those institutions participating within
Higher Education
23
• The Genetic Information Nondiscrimination Act (GINA)
24
• The General Data Protection Regulation (GDPR) in the European Union
25
• State laws setting standards for privacy and security such as the California Consumer Privacy
Act (CCPA)
26
• Minimum Acceptable Risk Standards for exchangers
27
• Federal Information Security Modernization Act (FISMA) requirements as incorporated into federal
contracts and research grants through agencies such as the National Institutes of Health (NIH)
28
Changes to the Stark Law physician self-referral regulations and the related anti-kickback statute took
effect in January 2021. These protect the donation of cybersecurity technology and services that are
“necessary and used predominantly to implement, maintain, reestablish effective cybersecurity.”
29
IT Assets Used by Large Organizations
Large organizations support their operations with complicated ecosystems of IT assets. All assets may
have cybersecurity vulnerabilities and are susceptible to cyber threats. There are three important
factors in securing assets: (1) understanding their relationship within your organization’s IT ecosystem,
(2) understanding how the workforce leverages and uses the assets, and (3) understanding the data
generated, stored, and processed within those assets.
19 “PCI DSS v4.0 Resource Hub,” PCI Security Standards Council, https://www.pcisecuritystandards.org/.
20 “Fact Sheet: SAMHSA 42 CFR Part 2 Revised Rule,” SAMHSA, https://www.samhsa.gov/newsroom/press-
announcements/202007131330.
21 “Gramm-Leach-Bliley Act,” FTC, https://www.ftc.gov/business-guidance/privacy-security/gramm-leach-bliley-act.
22 “Fraud & Abuse Laws,” HHS Ofce of Inspector General, https://oig.hhs.gov/compliance/physician-education/fraud-
abuse-laws/#:~:text=The%20Physician%20Self%2DReferral%20Law%2C%20commonly%20referred%20to%20
as%20the,relationship%2C%20unless%20an%20exception%20applies.
23 “Family Educational Rights and Privacy Act (FERPA),” US Department of Education, https://www2.ed.gov/policy/gen/
guid/fpco/ferpa/index.html.
24 “Genetic Information,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/special-topics/genetic-information/
index.html.
25 “General Data Protection Regulation: GDPR,” Intersoft Consulting, https://gdpr-info.eu/.
26 “California Consumer Privacy Act (CCPA),” State of California Department of Justice, https://oag.ca.gov/privacy/ccpa.
27 “Minimum Acceptable Risk Standards for Exchanges (MARS-E) 2.0,” HHS Guidance Portal, https://www.hhs.gov/
guidance/document/minimum-acceptable-risk-standards-exchanges-mars-e-20.
28 “4.1.9 Federal Information Security Management Act,” NIH, https://grants.nih.gov/grants/policy/nihgps/html5/
section_4/4.1.9_federal_information_security_management_act.htm.
29 The Stark Law, 42 C.F.R. § 411.357(bb)(1) and the Anti-Kickback Statute, 42 C.F.R. § 1001.952(jj) are the result of the
CMS Final Rule at 85 Fed. Reg. 77,492 (December 2, 2020).

Cybersecurity Pracces at Large Healthcare Organizaons
7Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Not all assets are equally important. Some are mission critical and must always be fully operational, while
others are less critical, and might even be ofine for days or weeks without harming your organization’s
mission or causing impact to patient safety. Some assets have large repositories of sensitive data that
represent signicant risk that are not necessarily critical to the enterprise’s business. In all cases,
organizations use IT assets for business reasons and should protect those assets with proper cyber
hygiene controls.
Examples of assets found in large organizations include, but are not limited to, the following:
• Devices used by the workforce that enable internet connectivity, such as mobile phones, tablets, voice
recorders, and laptop computers for dictation.
• Personal devices creating or maintaining sensitive data, often referred to as BYOD.
• Large deployments of IoT assets, including smart televisions, networked medical devices, printers,
copiers, security cameras, refrigeration sensors, blood bank monitoring systems, building
management sensors, and more.
• Data that includes IIHI stored and processed on devices, servers, applications, and the cloud.
This data could include names, medical record numbers, birth dates, SSNs, diagnostic conditions,
prescriptions, and mental health, substance abuse, or sexually transmitted disease information.
IIHI about a patient that is created or maintained by a HIPAA covered entity is PHI that must be
safeguarded against unauthorized use or disclosure.
• Assets related to the IT infrastructure, such as rewalls, network switches and routers, Wi-Fi
networks (corporate and guest), servers supporting IT management systems, and le storage systems
(cloud-based or onsite).
• Applications or information systems that support business processes. These can include ERPs,
pathology lab systems, blood bank systems, medical imaging systems, pharmacy systems (retail and
specialized), revenue cycle systems, supply chain or materials management systems, specialized
oncology therapy systems, radiation oncology treatment systems, data warehouses (clinical, nancial,
research), vendor management systems, and more.
8Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Document Guide: Cybersecurity Pracces
This volume provides medium-sized and large organizations with a series of cybersecurity practices
to prevent, react to, and recover from the ve cybersecurity threats identied in Table 1 below and
discussed in the Main Document (See the Main Document for detailed denitions and descriptions of
each threat).
Table 1. Five Prevailing Cybersecurity Threats to Healthcare Organizations
Threat Potenal Impact of Aack
Social engineering Malware delivery or credential attacks. Both attacks further
compromise your organization.
Ransomware attack Information system assets locked and held for payment of ransom
(extortion). Disrupts normal healthcare operations. Prevents business
functions like electronic billing for treatment services. May lead to
a breach of sensitive information and patient identify theft, as bad
actors have started exporting data and publishing it as part of the
extortion strategy.
Loss or theft of
equipment or data
Breach of sensitive information. May lead to patient identity theft.
Insider, accidental or
malicious data loss
Removal of data from your organization (intentionally or
unintentionally). May lead to a breach of sensitive information. May
also lead to patient identify theft.
Attacks against network
connected medical devices
Undermined patient safety, delay or disruption of treatment,
and well-being.
Each cybersecurity practice responding to the threats listed above is broken up into three core segments:
Sub-Practices for Medium-Sized Organizations (or medium sub-practices), Sub-Practices for Large
Organizations (or large sub-practices) and the Threats Mitigated by the practice. Each practice also
contains a series of suggested metrics to measure the effectiveness of the cybersecurity practice.
Medium sub-practices apply to both medium-sized and large organizations. Large sub-practices
are designed for application by large organizations. These large sub-practices could also benet an
organization of any size that has an interest in adopting them.
The following tables present summaries of each of the cybersecurity practices described herein.

Document Guide: Cybersecurity Practices
9Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
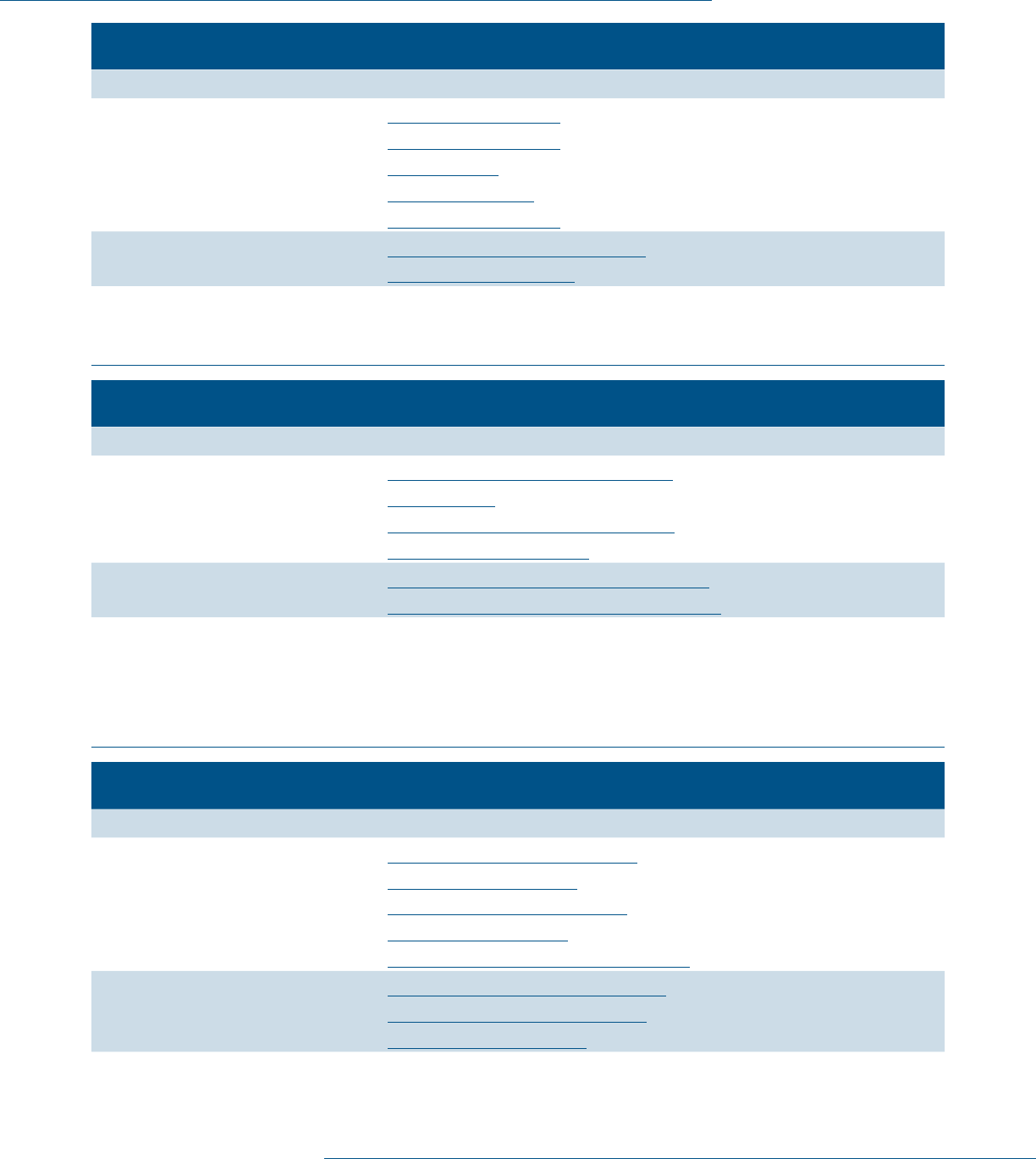
Cybersecurity Pracce 1: Email Protecon Systems
Assets Affected Sensitive Data, System Integrity
Medium Sub-Practices
1.M.A Basic Email Protection Controls
1.M.B Multi-Factor Authentication for Remote Access
1.M.C Email Encryption
1.M.D Workforce Education
Large Sub-Practices
1.L.A Advanced and Next-Generation Tooling
1.L.B Digital Signatures
1.L.C Analytics Driven Education
Key Mitigated Risks • Social engineering
• Ransomware attacks
• Insider, accidental or malicious data loss
Cybersecurity Pracce 2: Endpoint Protecon Systems
Assets Affected Sensitive Data, System Integrity, System Availability
Medium Sub-Practices
2.M.A Basic Endpoint Controls
2.M.B Mobile Device Management
Large Sub-Practices
2.L.A Automate the Provisioning of Endpoints
2.L.B Host Based Intrusion Detection/Prevention Systems
2.L.C Endpoint Detention Response
2.L.D Application Allowlisting
2.L.E Micro-Segmentation/Virtualization Strategies
Key Mitigated Risks • Ransomware attacks
• Loss or theft of equipment or data
Cybersecurity Pracce 3: Identy and Access Management
Assets Affected Sensitive Data Information Systems
Medium Sub-Practices
3.M.A Identity
3.M.B Provisioning, Transfers, and Deprovisioning Procedures
3.M.C Authentication
3.M.D Multi-Factor Authentication for Remote Access
Large Sub-Practices
3.L.A Federated Identity Management
3.L.B Authorization
3.L.C Access Governance
3.L.D Single Sign-On
Key Mitigated Risks • Ransomware attacks
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety
Document Guide: Cybersecurity Practices
10Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce 4: Data Protecon and Loss Prevenon
Assets Affected Passwords, PHI
Medium Sub-Practices
4.M.A Classication of Data
4.M.B Data Use Procedures
4.M.C Data Security
4.M.D Backup Strategies
4.M.E Data Loss Prevention
Large Sub-Practices
4.L.A Advanced Data Loss Prevention
4.L.B Mapping of Data Flows
Key Mitigated Risks • Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
Cybersecurity Pracce 5: IT Asset Management
Assets Affected Passwords, PHI
Medium Sub-Practices
5.M.A Inventory of Endpoints and Servers
5.M.B Procurement
5.M.C Secure Storage for Inactive Devices
5.M.D Decommissioning Assets
Large Sub-Practices
5.L.A Automated Discovery and Maintenance
5.L.B Integration with Network Access Control
Key Mitigated Risks • Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety
Cybersecurity Pracce 6: Network Management
Assets Affected PHI
Medium Sub-Practices
6.M.A Network Proles and Firewalls
6.M.B Network Segmentation
6.M.C Intrusion Prevention Systems
6.M.D Web Proxy Protection
6.M.E Physical Security of Network Devices
Large Sub-Practices
6.L.A Additional Network Segmentation
6.L.B Network Analytics and Blocking
6.L.C Network Access Control

Document Guide: Cybersecurity Practices
11Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce 6: Network Management
Key Mitigated Risks • Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety
Cybersecurity Pracce 7: Vulnerability Management
Assets Affected PHI
Medium Sub-Practices
7.M.A Host/Server Based Scanning
7.M.B Web Application Scanning
7.M.C System Placement and Data Classication
7.M.D Patch Management, Conguration Management
7.M.E Change Management
Large Sub-Practices
7.L.A Penetration Testing
7.L.B Vulnerability Remediation Planning
7.L.C Attack Simulation
Key Mitigated Risks • Ransomware attacks
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety
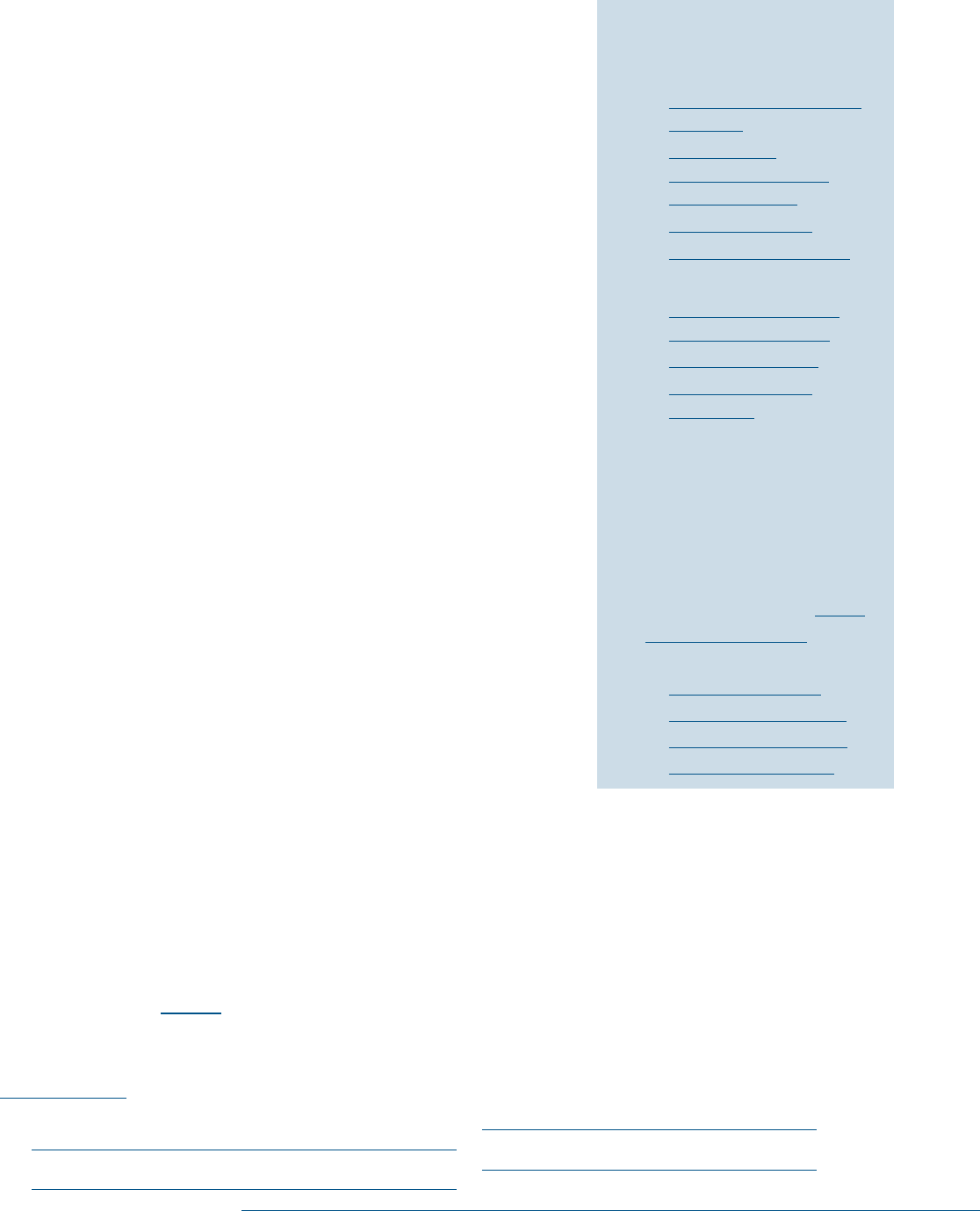
Cybersecurity Pracce 8: Security Operaons Center and Incident Response
Assets Affected PHI
Medium Sub-Practices
8.M.A Security Operations Center
8.M.B Incident Response
8.M.C Information Sharing and ISACs/ISAOs
Large Sub-Practices
8.L.A Advanced Security Operations Center
8.L.B Advanced Information Sharing
8.L.C Incident Response Orchestration
8.L.D Baseline Network Trafc
8.L.E User Behavior Analytics
8.L.F Deception Technologies
Key Mitigated Risks • Social engineering
• Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety

Document Guide: Cybersecurity Practices
12Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce 9: Network Connected Medical Devices
Assets Affected PHI
Medium Sub Practices
9.M.A Medical Device Management
9.M.B Endpoint Protections
9.M.C Identity and Access Management
9.M.D Asset Management
9.M.E Vulnerability Management
9.M.F Contacting the FDA
Large Sub-Practices
9.L.B Security Operations and Incident Response
9.L.C Procurement and Security Evaluations
Key Mitigated Risks • Attacks against network connected medical devices that may affect
patient safety
Cybersecurity Pracce 10: Cybersecurity Oversight and Governance
Assets Affected N/A
Medium Sub-Practices
10.M.A Policies
10.M.B Cybersecurity Risk Assessment and Management
10.M.C Security Awareness and Training
Large Sub-Practices
10.L.A Cyber Insurance
Key Mitigated Risks • Social engineering
• Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect
patient safety
13Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #1:
Email Protecon Systems
Areas of Impact
Sensitive Data, System Integrity
Medium Sub-Practices
1.M.A Basic Email Protection
Controls
1.M.B Multi-factor
Authentication for
Remote Access
1.M.C Email Encryption
1.M.D Workforce Education
Large Sub-Practices
1.L.A Advanced and Next-
Generation Tooling
1.L.B Digital Signatures
1.L.C Analytics Driven
Education
Key Threats Addressed
• Social engineering
• Ransomware attacks
• Insider, accidental, or
malicious data loss
405(d) Resources
• Prescription Poster: Email
Protection Systems
• Five Threats Flyers:
¡ Social Engineering
¡ Ransomware Attacks
¡ Insider, Accidental or
Malicious Data Loss
According to the 2021 Verizon Data Breach Investigations Report,
phishing was “present in 36% of breaches (up from 25% last year).”
Additionally, 23% of malware was delivered through email.
30
Phishing
isn’t the only social engineering threat to be concerned with. There
has also been a rise in Business Email Compromise (BEC) attacks,
whereby scammers attempt to trick business and individuals to
perform fraudulent wire transfer payments.
31
Though other areas of
signicant threat exist (including in the web application space), the
effectiveness of phishing attacks allows attackers to bypass most
perimeter detections by “piggy backing” on legitimate workforce
users. If an attacker obtains an employee’s password through any
type of social engineering attack, and if that employee has remote
access to your organization’s IT assets, the attacker has made
signicant progress toward penetrating your organization.
The two most common phishing methods are credential theft
(leveraging email to conduct a credential harvesting attack on
your organization) and malware dropper attacks (email delivery
of malware that can compromise endpoints). An organization’s
cybersecurity practices must address these two attack vectors.
Because both attack types leverage email, email systems should be
the focus for additional security controls.
Sub-Practices for Medium-
Sized Organizations
1.M.A: Basic Email Protection Controls
NIST Framework Ref: ID.RA-2, PR.AC-4, PR.AC-1, PR.AC-7, PR.DS-2, PR.PT-3, DE.CM-4
Standard phishing detection, antispam, and antivirus (AV) ltering controls are basic protections that
should be implemented in any email system. They are implemented directly on the email platform.
These controls assess inbound and outbound emails from known malicious senders or patterns of
malicious content. Table 2 below provides a list of suggested security implementations for email
protection controls.
30 “2021 Data Breach Investigations Report,” Verizon (2021), 56, https://www.verizon.com/business/resources/
reports/2021/2021-data-breach-investigations-report.pdf.
31 “2021 Data Breach Investigations Report,” Verizon (2021), 25, https://www.verizon.com/business/resources/
reports/2021/2021-data-breach-investigations-report.pdf.

Cybersecurity Pracce #1: Email Protecon Systems
14Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 2. Email Protection Controls
Control Descripon
Real-time deny
list
32
Community-based lists of IP addresses and host names of known or potential
spam originators. Consider lists provided by Spamhaus, Spamcop, DNSRBL, or by
your email vendor.
Distributed
Checksum
Clearinghouse
(DCC)
The DCC is a distributed database that contains a checksum of messages. Email
messages go through a checksum algorithm and then checked against the
database. Depending upon the threshold of checksum matches, these can be
determined to be spam or malicious messages.
Removal of open
relays
Open relays are Simple Mail Transfer Protocol (SMTP) servers that enable the
relay of third-party messages. SMTP is critical for the delivery of messages, but
you must congure it to allow messages only from trusted sources. Failure to do
this may permit a spammer or hacker to exploit the “trust” of your mail server to
transmit malicious content.
Spam/virus check
on outbound
messages
Spam/virus checks on outbound emails can detect malicious content, revealing
compromised accounts and potential security incidents. Review email spam/
virus rules as part of Cybersecurity Practice #8: Security Operations Center and
Incident Response.
AV check Scan all email content against an AV engine with up-to-date signatures. If
possible, this control should unpack compressed les (such as zip les) to check for
embedded malware.
Restrict the “Send
as” permission for
distribution lists
Limit distribution lists to essential members. Distribution lists can enable
attackers to disseminate malicious content from a compromised account.
Therefore, they and should not be accessible to large numbers of users.
Implement sender
policy framework
(SPF) records
A Sender Policy Framework (SPF) record identies which mail servers’ policy
framework (SPF) may send email on behalf of your domain. This enables the
receiving mail records server to verify the authenticity of the sending mail server.
This should be congured as part of a Domain-based Message Authentication
Reporting and Conformance (DMARC) record.
Implement domain
key identied mail
(DKIM)
DKIM is a method of email authentication that uses cryptography to ensure that
email messages come from authorized email servers. A public key is stored within
your organization’s domain name system (DNS) as a text (txt) record. All messages
sent from that domain are digitally signed with a DKIM signature that can be
validated through the DNS public key txt record. This should be congured as part
of a DMARC record.
32 Murthy Raju, “Using RBL and DCC for Spam Protection,” Linux.com (Last modied June 14, 2007), https://www.linux.
com/news/using-rbl-and-dcc-spam-protection.
Cybersecurity Pracce #1: Email Protecon Systems
15Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Control Descripon
Implement domain-
based message
authentication
reporting and
conformance
(DMARC)
33
DMARC is an authentication technology that leverages both SPF and DKIM based
message to validate an email’s From: address (i.e., the sender). DMARC enables
the receiving mail system to check SPF and DKIM records, ensuring conformance
reporting to the sending host as well as the “From:” address. It instills trust that
the sending party’s email address is not spoofed; spoong is a common attack type
used to trick users into opening malicious emails.
In most cases, email protection controls do not operate alone. When combined to evaluate an
organization’s emails, they contribute information that provides a more complete assessment of each
message. Modern systems score email content on each pass through the protection controls.
Organizations should implement this scoring technique and set at least three thresholds: OK for Delivery,
Quarantine, or Block/Drop. Each email should be scored to determine which of the three thresholds
applies. Based on that threshold, automated actions should be executed. Emails cleared for delivery
automatically pass through for additional processing. The email protection system discards Block/Drop
emails, and the user never sees them. Quarantine actions allow the user to evaluate the message in a
secured environment (not the user’s regular email box) for nal verication. In most cases, the system
delivers quarantined messages to the user daily in a single email digest for verication.
Adding X-Headers to the delivery of email messages is a good way to ag potential spam or malicious
email before sending it to the user. There are two common methods to accomplish this:
34
• Spam X-Header: If a message receives a score that prevents the system from denitively classifying
it as spam/malicious, the system can tag the message with an X-Header. The system modies the
subject or the top of the body of the message to include a [POSSIBLE SPAM] tag. This advises the
user to verify whether a message is legitimate prior to opening it.
• External Sender X-Header: Another common practice is to add an [EXTERNAL] tag to inbound
messages from external senders. The tag can be congured to be highly visible, such as “WARNING:
Stop. Think. Read. This is an external email.” This method is effective at identifying messages that
might be spoofed or faked to appear to have come from within your organization. It also informs the
email recipient to be cautious when clicking links or opening attachments from these sources. If you
leverage DMARC, you might consider exempting the External Sender X-header tag for messages
sent on behalf of your organization (e.g., hosted human resources [HR] systems) that pass DMARC
authentication. This may help email users understand the trust environment and identify when it
is necessary to be extra vigilant. Additionally, you may want to consider exempting messages from
other trusted partners to avoid alert fatigue.
Messages can also be marked (or digitally signed) when they originate from approved hosting or cloud-
based services with a legitimate need to spoof an internal address. This is common for communications
platforms, such as marketing systems, emergency management communications systems, or alert
management systems.
33 KC Cross, Denise Vangel, and Meera Krishna, “Use DMARC to Validate Email in Ofce 365,” Microsoft TechNet, (Last
modied October 8, 2017), https://technet.microsoft.com/en- us/library/mt734386(v=exchg.150).aspx.
34 KC Cross and Denise Vangel, “Congure Your Spam Filter Policies,” Microsoft TechNet, (Last modied December 13,
2017), https://technet.microsoft.com/en- us/library/jj200684(v=exchg.150).aspx.
Cybersecurity Pracce #1: Email Protecon Systems
16Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
1.M.B: Multi-Factor Authentication for Email Access
NIST Framework Ref: PR.AC-7
It is common and expected to share sensitive information through email systems. Email is the primary
mechanism used by most organizations to communicate electronically. It is also common to access email
remotely, as the workforce has become increasingly mobile.
Given the prevalence of credential harvesting attacks, if email systems are available, passwords are the
only controls prohibiting malicious users from accessing sensitive information within transmitted emails.
This is a critical exposure that increases organizations’ susceptibility to phishing attacks.
As discussed in Cybersecurity Practice #3: Identity and Access Management, two-factor authentication,
or multi-factor authentication (MFA), is the process of verifying a user’s identity through more than one
credential. The most common method is to leverage a soft token in addition to a password. The soft
token is a second credential that can be delivered through a mobile phone or tablet, devices that most
people have nearby. For example, the soft token could consist of a text message containing a code, or of
an application installed on a smartphone that provides the code and/or asks for independent verication
after a successful password entry.
Implementing MFA on the email platform mitigates compromised credential (i.e., user password)
risk. With MFA, a hacker requires both the smartphone and the user’s password, which signicantly
reduces the likelihood of a successful attack. MFA has proven to be an effective control to protect an
organization’s data from unauthorized access.
When implementing MFA, make sure to ensure all protocols used are multifactored. A common method
for delivering email to mobile devices is to support Post Ofce Protocol (POP3) and Internet Message
Access Protocol (IMAP) protocols. Unfortunately, these legacy protocols generally do not allow for MFA.
As with the email provider, if these protocols are to be used, they must allow them to be accessible by
only a single factor, generally the username and password. This back door can allow bad actors to access
your email systems that might have MFA protection on the “front door.” Be sure to switch over to the
usage of modern email authentication, which allows all mobile and desktop clients to leverage MFA and
disable these legacy authentication protocols.
1.M.C: Email Encryption
NIST Framework Ref: PR.DS-2
Email is the most common method of communicating content, including sensitive information, among
members of an organization. Although email might not be the preferred communication method, one
must assume that users will leverage this common and easy-to-use communication channel.
Email encryption is an important security protection. Multiple encryption techniques exist, though the
most common use third-party applications to conduct encryption, invoking them by tagging outbound
messages in some form. For example, tagging can occur by putting a trigger in the subject line (e.g.,
#encrypt, #condential), or the email client itself can invoke the third-party application. The techniques
used depend upon the technology solution deployed. By encrypting the envelope, you can ensure that no
matter where the email is forwarded, it will maintain its encrypted status. This level of protection is more
robust than implementing only transport layer security (TLS) protection for the message in transit.
Cybersecurity Pracce #1: Email Protecon Systems
17Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
When organizations have established partnerships with third-parties, fully encrypted, transparent email
delivery can be provisioned between the two entities’ email systems. Each system can be congured
to require TLS encryption when sending or receiving messages from the other. This ensures that the
messages are delivered over the internet in a manner that prevents their interception.
Whichever encryption technique is implemented, an organization’s workforce must be trained to use the
technique when transmitting sensitive information. This cybersecurity practice can be integrated into
the data protection cybersecurity practices discussed in Cybersecurity Practice #4: Data Protection and
Loss Prevention. Messages that users fail to encrypt can be automatically encrypted or simply blocked.
1.M.D: Workforce Education
NIST Framework Ref: PR.AT-1
While an organization can reduce its susceptibility to phishing attacks, it cannot eliminate the risk. Given
that phishing is one of the most common methods of attack and initial compromise, a layered defense
strategy is important.
Organizations should implement security awareness programs that provide context around email-based
attacks. The challenge presented to security departments is how to deliver concise educational and
awareness materials for spotting social engineering or phishing attacks when the workforce’s knowledge
level does not match the hacker’s level of sophistication. For example, it is easy to make a phishing email
appear to originate from the company itself, incorporating logos, department names, and management
names, but it is difcult to train an organization’s entire workforce to detect that fake message.
When implementing cybersecurity training programs, consider some of the key techniques outlined in a
2015 HBR article by Keith Ferrazzi:
35
• Ignite each manager’s passion to coach their employees: Engage and train the management
team. Leverage them to communicate security practices and information to staff in all areas of
your organization.
• Deal with the short shelf life of learning and development needs: Security information changes
continuously. Implement continuous and ongoing campaigns to maintain awareness of current
trends, issues, and events.
• Teach employees to own their career development: Customize cybersecurity training to the needs
of employees in different positions or units in your organization. Develop training techniques and
awareness materials that are relevant to the workforce member’s role and access.
• Provide exible learning options: Provide options, including on-demand and mobile training solutions,
that allow the workforce to schedule and complete training independently.
• Serve the learning needs of virtual teams: Recognize that many workforce members work remotely
and virtually. Training solutions should t within the work environment of virtual employees.
• Build trust in organizational leadership: Leaders must be open and transparent; to lead by example.
Managers must demonstrate to the workforce that they are fully engaged in security strategy and
committed to successful execution of security controls and techniques.
35 Keith Ferrazzi, “7 Ways to Improve Employee Development Programs,” Harvard Business Review (Last modied July
31, 2015), https://hbr.org/2015/07/7-ways-to-improve-employee-development-programs.
Cybersecurity Pracce #1: Email Protecon Systems
18Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Match different learning options to different learning styles: Effective training accommodates the
different learning styles and requirements of workforce members who function in diverse work
environments within a single organization. Consider multiple options for conducting each training
course to maximize training effectiveness and efciency.
Organizations should implement multi-faceted training campaigns that engage users to catch phishing
and other social engineering attempts through multiple channels. Points to include in a successful training
campaign include:
• Sender verication: Users should examine very carefully the sender of the email message. It is
common to spoof an organization’s name by changing a simple character, for example, “google.c0m”
rather than “google.com.” Educate users to be on the lookout for emails where your organization’s
name appears with a separate email domain, such as “!CME.google.com” rather than “acme.com.”
• Follow the links: Every link in an email message is suspect. Organizations should limit the use of links
in corporate messages to those that are necessary. Users should hover the cursor over each link
to check the corresponding Uniform Resource Locator (URL) and determine whether it is credible.
Specically, mismatched URLs (i.e., those where the name of the link in the email does not match
the corresponding URL) are highly suspect. This may not be effective when URLs are rewritten by a
security tool to facilitate malicious URL blocking. This process is described in 1.L.A: Advanced and
Next-Generation Tooling under URL click protection via analytics.
• Beware of attachments: Though it can be difcult to determine whether an attachment is malicious
based on the content of an email message, there are often clues. Be wary of messages that require
immediate action, for example, “You must read this right away.” Be cautious when receiving
attachments from senders with whom you do not regularly correspond. It is important to detect
malicious attachments, which may contain malware or exploit scripts that permanently compromise
your computer. Avoid enabling macros or running executables to view attachment content.
• Suspect content: In most cases, hackers entice recipients of email to follow a link or open an
attachment. They will use messages to play with the natural curiosity and emotions of those
receiving the email. These messages vary widely from urgent messages such as, “Your account will be
deactivated unless you re-register,” to scary messages such as, “The IRS is suing you and you must ll
out the attached form.” Hackers also prey on hopes and desires. Examples of these messages include,
“You have won a $100 Amazon gift card!” and the well-known “Nigerian Prince” messages.
• Avoid acting: BEC schemes typically encourage the recipient to take an action (e.g., completing a
wire transfer). These messages may impersonate a senior executive or key vendor/supplier. In
many cases, they may require a quick action to avoid a penalty, lost deal, etc. In all cases, changes to
account numbers, wire transfers, requests to send sensitive information (e.g., W2 data) should be
conrmed by verifying the sender based on known contact information—not based on the contact
details delivered in the malicious email.
As an organization develops its awareness campaigns, keep this simple goal in mind: empower the
user community to be “human sensors”. Detection of malicious activity and reporting these incidents
to the appropriate cybersecurity personnel is crucial. As the saying goes, “If you see something, say
something.” The earlier cybersecurity personnel become aware of a phishing attack or social engineering
campaign, the faster they can execute Cybersecurity Practice #8: Security Operations Center and
Incident Response.
Cybersecurity Pracce #1: Email Protecon Systems
19Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
The following are recommended channels for cybersecurity awareness campaigns:
• Email Click Button: Add a button to the email client that allows for automated reporting of a
suspicious email. This reporting can be congured to go directly to your organization’s cybersecurity
department and can increase the likelihood your workforce will report suspect messages. The
cybersecurity department should maintain a routine procedure for processing any suspicious emails
provided to them. For more specics, review Cybersecurity Practice #8: Security Operations
Center and Incident Response.
• Monthly phishing campaigns: The most effective means of training the workforce to detect a
phishing attack is to conduct simulated phishing and social engineering campaigns. The authorized
cybersecurity personnel or third-party provider crafts and sends phishing emails to users with email
accounts. These emails have embedded tracking components (e.g., to track link clicks). Tracking
enables your organization to identify employees who detect the email as a phishing attack and those
who fail to detect the attack, opening the email or clicking the emailed links. Your organization can
then provide the appropriate training and feedback as soon as possible after the event. Simulated
phishing attacks provide a cause-and-effect training opportunity and is incredibly effective. Consider
conducting phishing simulations on at least a monthly basis for the entire workforce. Develop
specialized simulations for higher-risk areas within your organization. These could be based on the
department (such as nance and HR) or on data identifying your highest-risk users. Phishing and
social engineering campaigns should track (and potentially reward) users that successfully report the
test message.
• Ongoing and targeted training: Organizations should include phishing content in ongoing privacy and
security training. Targeted training should be provided to users that experience a high failure rate
when presented with a simulated phishing email. Another group that should be provided specic
training includes those “high-value assets” of spear phishing targeted attacks such as leadership,
management, and other employees with nancial responsibilities.
• Departmental meetings: Hold departmental meetings to disseminate information on cybersecurity
events and trends. Brief presentations or informal conversations provide face-to-face context and
build relationships between cybersecurity personnel and your organization’s workforce. These
relationships encourage a continuous dialogue that elevates the visibility of cybersecurity across
your organization.
• Email campaigns: Deliver a pointed email message or alert about specic attacks. Provide Secure
Multipurpose Internet Mail Extensions (S/MIME) or other digital certicates as evidence that these
messages are authentic. Remember that attackers will attempt to do the same thing!
• Newsletters: Working independently or with your organization’s marketing department, develop and
distribute a cybersecurity newsletter. Produce articles that explain how to catch a phishing attack or
social engineering campaign. Better yet, provide an example of an actual phishing email, highlighting
the warning signs that might have resulted in identifying the message as a fake, thereby preventing
the attack.
• Change Leader: Appoint a change leader to be responsible for internal organizational collaboration.
This change leader should look at the internal culture of your organization to determine if employees
feel condent on how, when and what to report as early collaboration and coordination can save time
and resources.

Cybersecurity Pracce #1: Email Protecon Systems
20Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Large Organizations
1.L.A: Advanced and Next-Generation Tooling
NIST Framework Ref: PR.DS-2, DE.CM-5, DE.CM-7
Many sophisticated solutions exist to help combat the phishing and malware incidents. These solutions
are called advanced threat protection services. They use threat analytics and real-time response capabilities
to provide protection against phishing attacks and malware.
The list below describes some of these tools:
• URL click protection via analytics: In a modern phishing attack, the hacker will create a web page on
the internet for harvesting credentials or delivering malware. Next, the hacker will conduct an email
campaign, sending emails with a link to a web page that does not have malicious content. Because
the linked page is not malicious, traditional spam and AV protections clear the email for delivery to
the user. As soon as the emails are delivered, the hacker will change the linked web page to the newly
created malicious web page. This allows the hacker to bypass many traditional email protections and
leaves your organization to rely on the user’s vigilance and awareness.
Protection technologies that rely on analytics leverage the ability to re-write links embedded in
an email message. The rewritten URLs point to secure portals that apply analytics to determine
the maliciousness of the request at the time of the click. Therefore, the message is protected no
matter where or when the user clicks the link. Such technologies use the cloud and numerous
sensors throughout the install base to check linked sites in real time. They can also block discovered
malicious sites ahead of time to inoculate your organization.
It is important to note that, as URL click protection tools will rewrite URLs embedded in emails, it will
be difcult for users to “hover” over the URL and determine if it is a legitimate source.
• Attachment sandboxing: Another common attack technique is to send attachments with embedded
malware, malicious scripts, or other local execution capabilities that compromise vulnerabilities on
the endpoint where the attachment is launched. These attachments bypass traditional signature-
based malware blocking by using multiple obfuscation techniques that alter the attachment’s content
to provide a different hashing signature.
Sandboxing technologies open attachments proactively in virtual environments to determine
what behaviors occur after the user opens the attachment. The protection system determines
whether a le is malicious based on these behaviors, such as system calls, registry entry creation, le
downloading, and others.
• Automatic response: Another useful technique is to implement mechanisms that automatically
rescind or remove email messages categorized as malicious after delivery to a user’s mailbox.
After using the analytics approach described earlier in this section to identify malicious emails,
cybersecurity response teams remove these messages from the user’s mailbox. This manual process
requires identifying the characteristics of the malicious email message, searching your organization’s
email environments, and deleting messages that match the identied characteristics. This time-
consuming process is difcult to run in a 24x7x365 operation and can miss malicious emails or
remove legitimate ones by mistake.

Cybersecurity Pracce #1: Email Protecon Systems
21Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
As an alternative to costly manual removal, automatic response technologies can identify the
signature of a delivered email. When advanced threat tools determine that a previously clean
message has become malicious, it can automatically delete that email message from all user
mailboxes in your organization. This reduces the labor involved compared with the manual processes
and provides the automation consistency.
• Imposter Protections: Another common tactic by bad actors is to create an email that has the same
name as a key leader within your organization, doing so within one of the free email systems such as
Gmail, Yahoo, Hotmail, and others. The bad actor will then send very targeted messages to specic
members inside your organization (usually initially without any malicious attachments or links),
with the goal of engaging in a dialogue and establishing some level of trust with the recipient. Once
the trust has been established the bad actor will then ask the recipient to take some type of action
on their behalf, such as purchasing one-time gift cards, changing bank account numbers, or even
providing user credentials. This is a very common tactic with BEC attacks. To protect against these
types of attacks, modern email defense tools can ag VIP users, such as the Chief Executive Ofcer
(CEO), Chief Financial Ofcer (CFO), Chief Operations Ofcer (COO), or even heads of research,
and take special precautions against any inbound messages from personal email accounts with these
names. This type of system does require some manual tuning and the ability to understand the VIPs
legitimate real personal account (to not create false positives). Such a control can effectively mitigate
targeted social engineering attacks.
1.L.B: Digital Signatures
NIST Framework Ref: PR.DS-2, PR.DS-6, PR.DS-8
Digital signatures allow a sender to leverage public/public key cryptography to cryptographically sign an
email message. This does not encrypt the message itself. Rather, it validates that a received message is
from a veried sender and has not changed in transit.
If trusted root certicates are used to create the S/MIME certicate used in digital signatures, most
modern email clients will check and provide verication automatically by presenting an icon on the
message itself. This icon is useful when training your workforce to determine the validity of an email.
Be careful! Many email protection technologies change the content of email messages (e.g., by tagging
subject lines, re-writing URLs). Digital signature technology that maintains the integrity of an email
will fail when you use these other protection techniques. Currently, there is no method to resolve
this problem.

Cybersecurity Pracce #1: Email Protecon Systems
22Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
1.L.C: Analytics-Driven Education
NIST Framework Ref: PR.AT-1
Cybersecurity departments use data and analytics from both regular email protection platforms and
advanced threat protection systems to identify the most frequently targeted users in an organization.
These users might not be the ones you think are highly susceptible, such as the CEO or the nance
workforce. With the systems discussed in this section, SOCs can identify targets, implement increased
protections (e.g., lower thresholds for spam/malware checking, delayed processing time for attachments),
and provide on-the-spot and targeted education. Informing these individuals of their high-risk prole
instills a heightened sense of awareness and increased vigilance. Data on the most successful types of
phishing messages can help drive greater awareness on the actual threat your organization faces.
Key Mitigated Threats
1. Social engineering
2. Ransomware attacks
3. Insider, accidental or malicious data loss
Suggested Metrics
• Number of malicious phishing attacks prevented on a weekly basis, compared to total email volume. The
goal is to ensure systems are working. Sudden changes in the rate of phishing attacks should trigger
operations to checks to ensure that systems are still operating as intended.
• Number of malicious URLs and email attachments discovered and prevented on a weekly basis, compared
to total email volume. The goal is to measure the effectiveness of advanced tools, like click protection
or attachment protection.
• Number of phishing attacks that bypassed your prevention systems and detected by end users on a
weekly basis. This measurement will provide a measurement to determine the effectiveness of your
preventative controls and identify room for improvement.
• Number of accounts compromised through phishing. This is based on users who accessed a malicious
website. It assumes that a registered click indicates compromised credentials, so be sure to change
the credential before further compromise can occur. Implement education to keep this number as
low as possible.
• Number of malicious websites visited on a weekly basis. The goal is to establish a baseline
understanding, then strive for improved awareness through education activities that train employees
to avoid malicious websites.
• Percentage of users in your organization who are susceptible to phishing attacks based on results of
internal phishing campaigns. This provides a benchmark to measure improvements to the workforce’s
level of awareness. The goal is to reduce the percentage as much as possible, realizing that it is
nearly impossible to stop all users from opening phishing emails. A secondary goal is to correlate
the percentage of susceptible users with the number of malicious websites visited or the number of
malicious URLs opened.

Cybersecurity Pracce #1: Email Protecon Systems
23Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Percentage of users who report suspected messages received during a phishing campaign. The more users
that ag suspicious messages, the greater the chance the SOC will be alerted and able to remove
messages that evaded technical controls. This is also can be used as a measure of user awareness.
• List of the top 10 targeted users each week, with corresponding activity. For example, how many
phishing emails do the top three users receive compared with the rest of the workforce? What
positions do these users hold in your organization? Are there correlations among the user, the user’s
position, and the number of phishing emails received? What inferences and conclusions are possible?
The goal is to conduct targeted awareness training to these individuals, advising them that they are
targets more often than other users, and increasing their vigilance as well as their ability to detect
and report phishing attacks.
• Average time to detect (mean time to detect) and average time to respond (mean time to respond)
statistics for phishing attacks on a weekly basis. Time to detect measures how long the phishing attack
was in progress before the cybersecurity department was aware of it. Response times measure of
how quickly the cybersecurity department neutralized the messages to end the attacks. Ideally, both
metrics should be as low as possible. Establish a baseline to understand the current state and set
goals to improve performance.
• Number of users sent internal campaign, percentage that never opened it, percentage that reported it, and
percentage that clicked. Of the number that clicked, what is the percentage that attempted to provide
credentials or download and run an executable le?

24Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #2:
Endpoint Protecon Systems
Areas of Impact
Passwords, PHI
Medium Sub-Practices
2.M.A Basic Endpoint Controls
2.M.B Mobile Device
Management
Large Sub-Practices
2.L.A Automate the
Provisioning of Endpoints
2.L.B Host Based Intrusion
Detection/Prevention
Systems
2.L.C Endpoint Detention
Response
2.L.D Application Allowlisting
2.L.E Micro-Segmentation/
Virtualization Strategies
Key Threats Addressed
• Ransomware attacks
• Loss or theft of equipment
or data
405(d) Resources
• Prescription Poster:
Endpoint Protection
Systems
Endpoints are the assets the workforce uses to interface with an
organization’s digital ecosystem. Endpoints include desktops,
laptops, workstations, and mobile devices. Current cyber-attacks
target endpoints as frequently as networks. Implementing
baseline security measures on these assets provides a critical
layer of threat management. As the modern workforce becomes
increasingly mobile, it is essential for these assets to interface and
function securely.
Endpoints are not static on a healthcare organization’s network.
Organizations commonly leverage virtual teams, mobility, and other
remote access methods. In some cases, endpoints rarely make it to
the corporate network. It is important to build cybersecurity hygiene
practices with these characteristics in mind.
36
Sub-Practices for Medium-
Sized Organizations
2.M.A: Basic Endpoint Protection Controls
NIST Framework Ref: PR.IP-1, PR.IP-12, PR.AC-4, PR.DS-1, DE.CM-4
Table 3 describes basic endpoint controls with practices to implement and maintain them.
Table 3. Basic Endpoint Controls to Mitigate Endpoint Risk
Control Descripon Implementaon Specicaon
Antivirus (AV) Technology capable
of detecting known
malicious malware
using signatures,
heuristics, and
other techniques.
• Push out AV packages using endpoint management
systems that interface with Windows and Apple
operating systems.
• Develop metrics to monitor the status of AV engines,
signature updates, and health.
• Dispatch eld services/desktop support for malware that is
detected but not automatically mitigated.
• Leverage network access control (NAC) to conduct a
validation check, prior to enabling network access.
36 “CIS Control 5: Secure Congurations for Hardware and Software on Mobile Devices, Laptops, Workstations and
Servers,” Center for Information Security Controls (Accessed September 24, 2018). https://www.cisecurity.org/
controls/secure-conguration-for-hardware-and-software-on-mobile-devices-laptops-workstations-and-servers/.

Cybersecurity Pracce #2: Endpoint Protecon Systems
25Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Control Descripon Implementaon Specicaon
Full disk
encryption
Technology capable
of encrypting an
entire disk to make
it unreadable
for unauthorized
individuals.
• Ensure encryption is enabled on new endpoints acquired
by your organization.
• Connect encryption management to endpoint
management systems that interface with mobile and
traditional operating systems.
• Develop metrics to monitor the status of encryption.
• Dispatch eld services/desktop support teams to resolve
encryption errors.
• Use anti-theft cable locks to lock down any device that
cannot support encryption.
• Leverage NAC to conduct a validation check prior to
enabling network access.
• Maintain audit trails of this encryption in case a device is
ever lost or stolen.
Hardened
baseline
images
Congure
the endpoint
operating system
in the most secure
manner possible.
• Enable local rewalls and limit inbound access to the
endpoint to only required ports.
• Disable weak authentication hashes (e.g., LANMAN, NTML
Version 1.0).
• Prevent software from auto-running/starting, especially
when using any directly connected USB device (e.g., a
thumb drive).
• Disable unnecessary services and programs.
• Permit usage only of known hardware encrypted any
directly connected USB device (e.g., a thumb drive) for
writing data.
• Review and consider the implementation of Security
Technical Implementation Guides.
37
Local
administrative
rights
The provisioning of
privileged access to
users for installing or
updating application
and OS software.
• Limit local administrative rights deployed to endpoints.
Use endpoint management systems to install new
programs and patch systems.
• For users that require administrative rights, deploy
a local account with administrative privileges that is
separate from the general user account. Never allow
a general user account to operate with administrative
privileges. Doing so increases vulnerability to malware and
client-side attacks.
37 “Security Technical Implementation Guides (STIGs),” Information Assurance Support Environment (IASE) (Accessed
September 24, 2018), https://public.cyber.mil/stigs/.

Cybersecurity Pracce #2: Endpoint Protecon Systems
26Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Control Descripon Implementaon Specicaon
Patching A process ensuring
regular patching
of endpoint OS
and third-party
applications.
• Establish an endpoint management system which
covers mobile and traditional network, desktop and
server devices and distribute OS patches during regular
maintenance times.
• Automatically update and distribute patches to third- party
applications that are known to be vulnerable, such as
internet browsers (e.g., Adobe Flash, Acrobat Reader, Java).
• Develop metrics to monitor patch status. Review on a
weekly basis.
• Dispatch eld services/desktop support for endpoints that
fail to patch.
• Systems often need to be rebooted before patching
takes effect.
• Organizations should reference Cybersecurity Practice
#9: Network Connected Medical Devices for additional
considerations for patching medical device rmware.
End-of-
Life (EOL)
Management
Operating systems,
software and
applications no
longer supported by
the vendor/provider
and do not receive
product updates and
security patches.
Use of these
products represents
a signicant risk
to your data,
information systems,
and overall mission.
Operating systems,
software and
applications that are
no longer supported
by the vendor/
provider should
be removed from
the environment.
When an operating system, software or application is
determined to have reached EOL or will reach EOL within
the upcoming year based on vendor notications and other
listings/sources, the risk must be mitigated in one of the
following ways:
1. Upgrade, retire or stop the use of an unsupported
operating system, software or application immediately by
the date specied in the extended support agreement or
the announcement by the vendor/provider.
2. When the removal or retirement of an unsupported
operating system, software or application is not
operationally feasible, the System Owner should attempt
to acquire additional support from the vendor. When
not feasible, your organization should follow their risk
acceptance/policy exception process to document
reasonable and appropriate mitigating controls and a
timeline for resolving the risk.

Cybersecurity Pracce #2: Endpoint Protecon Systems
27Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Control Descripon Implementaon Specicaon
Tap-n-Go
Authentication
Multi-factor, or
secondary factor,
authentication
systems that allow
users to log in to
their workstations
by “tapping”
their badge.
Requires the installation of a Tap-n-Go compatible system.
Consider the following:
1. Establish institutional Identities, as dened
within Cybersecurity Practice #3: Identity and
Access Management.
2. Tie an individual’s identity to the Tap-n-Go system.
3. Establish a reasonable timeout period (usually less
than 15-30 minutes) so the session can be ‘locked’
after inactivity.
4. Enable session persistence in the Tap-n-Go system,
so that when a user taps into a separate endpoint, the
session can migrate over in its current state.
Organizations should reference Cybersecurity Practice #5: IT Asset Management to determine whether
their endpoints meet IT asset management (ITAM) requirements. Examples include maintaining a proper
inventory of endpoints, reimaging endpoints as they are redeployed, and securely removing endpoints
from circulation when decommissioned.
When employees leverage personally owned devices (i.e., BYOD) that are not managed by your
organization, care should be taken to determine how these practices should be applied. If minimum
standards can’t be enforced by NAC (or similar mechanisms), a separate segmented network should be
provided for personal devices used to access your organization’s systems and applications.
Ensure workforce members are trained on the need to report any lost or stolen endpoints to your
organization’s cybersecurity department.. Reporting should occur promptly so the cybersecurity
department can execute the proper incident response (IR) procedures, outlined in Cybersecurity Practice
#8: Security Operations Center and Incident Response.
2.M.B: Mobile Device and Mobile Application Management
NIST Framework Ref: PR.AC-3
Mobile devices, such as smartphones and tablets, present their own management challenges. Multiple
security conguration options exist for these devices, and organizations should congure the devices
consistently to comply with organizational security policies.
38
Mobile device management (MDM) technologies manage the conguration of devices connected to the
MDM system. In addition to conguration management, they may offer application management and
containerization. Mobile application management (MAM) solutions are a type of containerization where
your organization can control where the application is installed, how it is congured, and aspects of
the device’s security (e.g., data encryption, biometric authentication). All three elements are important
to consider, especially for organizations that allow the use of personal devices in business operations.
38 “CIS Benchmarks,” Center for Information Security (Accessed September 24, 2018), https://www.cisecurity.org/cis-
benchmarks/.

Cybersecurity Pracce #2: Endpoint Protecon Systems
28Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
MAM works best where people may only need access to specic applications and offer exibility when
employees leverage their own devices in a BYOD environment.
Because most mobile devices travel on and off your organization’s network, it is important to consider
cloud-based MDM systems to enable consistent check-in. If cloud-based systems are not available, then
the onsite MDM systems must be accessible over the internet through virtual private network (VPN)
connectivity or in your organization’s demilitarized zone (DMZ). The list below further outlines the
capabilities of MDM systems.
• Conguration management: At minimum, ensure that passcodes are in place and encryption is
enabled. Be sure each device locks automatically after a predened duration (i.e., one minute).
Implement device wipe functions after a series of unsuccessful logins (i.e., 10 unsuccessful logins).
Limit the amount of time that an email can reside on the mobile device (i.e., 30 days maximum).
Consider leveraging an “Always on VPN” to protect the corporate device when users connect to
unsecured wireless networks. Also, consider prohibiting the installation of unsigned applications.
• Application management: Malicious applications reside in app stores and may appear to be legitimate
(e.g., PDF readers, Netix apps), when they really contain malicious code that provides access to data
elsewhere on the mobile device. MDM solutions use allowlisting or denylisting techniques to limit
the installation of these malicious applications. Consider both, especially for devices that run on the
Android platform (an open platform that accepts a wide range of applications).
• Containerization: Organizations with BYOD policies should consider containerization technologies,
such as MAM. These technologies segment and process business data on a mobile device separately
from personal data. Containerized business applications exist only in a hardened container on
the mobile device. Examples of such business applications include email, calendaring, and data
repositories. Containerization allows your organization to wipe the container and clear business
data from the device when the workforce member leaves or changes position in your organization. It
also limits the risk that personally downloaded malicious applications will access business data.
Sub-Practices for Large Organizations
2.L.A: Automate the Provisioning of Endpoints
NIST Framework Ref: PR.DS-5
It is challenging to manage thousands of endpoints consistently, especially when endpoint provisioning
processes are manually executed. Most organizations do not have the necessary resources to run such
an operation.
Value-added resellers (VARs) that sell endpoints through supply chains can precongure endpoints
before delivering them to an enterprise. To implement preconguring, your organization must build a
“gold image,” with a series of checklists and conguration procedures, and provide it to the VAR. This
approach helps to ensure a consistent and resilient deployment of endpoints. The image must be updated
periodically so new computers are deployed with the latest patches, agents, and other congurations.
There should also be a process for updating systems already deployed so they remain aligned with
current standards.

Cybersecurity Pracce #2: Endpoint Protecon Systems
29Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
In some cases, vendors provide the ability for an organization to provision devices centrally. For example,
Apple provides this service for its devices through its Device Enrollment Program (DEP). The DEP enables
an organization to simplify enrollment and endpoint security management. Your organization enters the
serial number or order number of the new device in the DEP, initiating a series of device conguration
tasks that are specic to your organization’s requirements. Further information is available in Apple’s
DEP Guide.
39
2.L.B: Host-Based Intrusion Detection and Prevention Systems
NIST Framework Ref: PR.DS-5
Host-based intrusion detection systems (HIDS) and Host-based intrusion prevention systems (HIPS) use
a protection method like network-based intrusion detection and prevention systems. These technologies
should be deployed on endpoints to detect patterns of attacks launched. Attacks can originate at the
endpoint’s network, or through client-side attacks that occur when using email or browsing the web.
HIDS and HIPS technologies are usually deployed and managed through central endpoint management
systems used to manage endpoint software and patching. Congure them to auto-update against their
command servers. The command servers should be congured to regularly download fresh signatures of
attack indicators.
2.L.C: Endpoint Detection and Response
NIST Framework Ref: PR.DS-5, RS.AN-1
Endpoint detection and response (EDR) technologies (also known as Advanced Threat Protection or
ATP) helps bridge the gap between execution and processing that occurs in an organization’s eet of
endpoints. These agent-based technologies utilize the continuous monitoring features provided by
anti-virus vendors and augment the data with analytical analysis and rules-based automated response.
These new features provide real-time response and mitigation for suspicious running processes, network
connections, le actions, and other irregular activities. Most of the major anti-virus vendors have updated
their offerings to include these added EDR analytical features and are highly recommended to enable
within an organization. Key features include:
• Analysis of newly installed processes and services.
• If malware is installed in your organization’s environment, cybersecurity professionals can “reach in
and remove” the malware from thousands of devices using a single action.
• Providing cybersecurity departments with forensic and analysis capabilities to search for suspicious
activities and supplement IR processes.
To ensure EDR implementation and use success, the following best practices/guidelines have
been gathered.
39 “DEP Guide,” Apple (Last modied October 2015), https://www.apple.com/business/site/docs/DEP_Guide.pdf.

Cybersecurity Pracce #2: Endpoint Protecon Systems
30Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Have a Plan
Review your current anti-virus solution to understand their EDR capabilities and what is needed to enable
the new features. If your current solution does not provide these new capabilities, carefully evaluate
which solution best meets your needs and organization. Consider the time for installation and support,
whether to use an in-house or managed EDR, how to best prevent threats to your organization, and nally
how to respond to threats. Primary components of a successful EDR implementation plan should include:
• Endpoint agent deployment: Endpoint agents conduct the real-time monitoring and data collection.
The data collection should include start/stop of processes, network connections, and data collection.
To minimize performance and the number of endpoint agents, it is highly recommended that these
features are enabled through your current anti-virus solution. The deployment of these agents
should be enforced for all endpoint assets during the build process.
• Automated response: Using pre-congured rules, EDR can respond to the threats and anomalous
behaviors real-time. The automated response can provide the opportunity to alert a SOC, disconnect
a user, or quarantine/delete a suspicious le. Initially, the plan should enable the EDR solution to
be entered into a ‘log-only’ or ‘notify’ conguration. As the product is deployed and gains data on
endpoints, the appropriate blocking and real-time automated response rules should be implemented.
• Forensic investigation and real-time analysis using analytics: Real-time analysis utilizes normal patterns
to create a security baseline. Once the baseline has been created, security events can be generated
for anomalous patterns as they occur outside the baseline. Forensic investigation tools provide an
analyst the capability to research past incidents and activity on the endpoint. Existing IR playbooks
should be updated to include these new forensic investigation capabilities. In addition to IR
playbooks, the forensic investigation capabilities should be implemented into daily hunting exercise
and threat intelligence reviews of indicators of compromise (IOCs).
Train and Educate
As EDR is deployed to endpoints, an appropriate training and education plan should be created for the
various roles that may be impacted. A specic training plan should be created for:
• Cybersecurity incident responders and hunters: EDR provides a vast knowledge of information related
to cybersecurity incidents. Develop a training plan for cybersecurity analysts to use the new features
to extend investigation to the endpoints. Training should also include IR steps and processes. An
understanding of the MITRE ATT&CK® framework will help the analyst to understand the various
attack methods and capabilities.
40
• Service or help desk analysts: As the agent is deployed to the various endpoints, the device may
experience some negative impact to applications or endpoint performance. Service or help desk
analysts need to be aware the type of calls that may come into the service desk and the steps to
remediate these problems. Additionally, if the endpoint user is notied of a security event, the
service desk employee needs to be aware to quickly escalate the call to the appropriate IR team.
• Client eld services team: Endpoint IT support techs need to be aware of the new technologies and
how to support reported endpoint errors. They should also be aware of the various IR touchpoints
and escalation steps.
40 MITRE ATT&CK® (Accessed May 26, 2022), https://attack.mitre.org/.

Cybersecurity Pracce #2: Endpoint Protecon Systems
31Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Assess All Permissions and Access Codes
Social engineering is still one of the most dangerous threats to enterprise security today. It is important
to implement appropriate segregation of duties and rights to maintain the installation and removal of the
EDR agent. Congure a password or PIN that must be entered to remove or disable the EDR software.
This removal password should not be shared or provided to the endpoint user. This also minimizes the
risk to malicious software that will rst try to disable the software before infection.
Monitor 24/7
Be sure to integrate the events from the EDR into your security incident and event management (SIEM)
and security operation center. Remember to constantly collect and analyze the security data you need.
Remember that EDR stands for endpoint detection and response. It involves detecting and responding
to threats, which means it must be both proactive and reactive. Proactive EDR is focused on nding and
preventing attacks before they happen. Alternatively, if an attacker does get into your network, it’s time
for reactive EDR.
Use EDR as a Complement
Using EDR as a complement to other security applications strengthens the overall protection of your
organization to an attack. Numerous network security services and vendors exist today. EDR security is a
tool to enhance your enterprise’s defenses, but it’s not the only thing you need. Make sure you have a full
lineup of network security features, including AV, rewalls, patch management, and others.
2.L.D: Application Allowlisting
NIST Framework Ref: ID.AM-2, PR.DS-6
Application allowlisting technologies permit only applications that are known and authorized to run,
rather than identifying applications that not permitted to run. These technologies assume it is impossible
to identify and denylist (or block) every malicious application, so all applications are blocked except those
that are allowlisted. In concept, this is application-level zero trust.
Application allowlisting can be based on a variety of application le and folder attributes, including
the following:
• File path: This is the most general attribute to permit all applications contained within a particular
path (directory/folder). Used by itself, this is a very weak attribute, because it allows any malicious
les placed within the directory to be executed. However, this attribute becomes stronger if the
path is protected by strict access controls that only allow authorized administrators to add or modify
les. Paths can be benecial by not requiring each le within the path to be listed separately, which
reduces the need to update the allowlist for every new application and patch.
• Filename: The name of an application le is too general to be used on its own. If a le were to become
infected or be replaced, its name would be unchanged so the le would still be executed under the
allowlist. Also, an attacker could simply place a malicious le onto a host and use the same name as
a common benign le. Because of these weaknesses, this attribute should not be used on its own;
rather, it should be paired with other attributes. For example, it would be stronger to combine path
and lename attributes with strict access controls or to combine a lename attribute with a digital
signature attribute (described below).
Cybersecurity Pracce #2: Endpoint Protecon Systems
32Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• File size: This is typically only used in combination with other attributes, such as lename.
Monitoring the le size assumes that a malicious version of an application would have a different le
size than the original; however, attackers can craft malicious les to have the same length as their
benign counterparts. Other attributes, such as digital signature and cryptographic hash, provide
substantially better unique identication of les than le size does, and should be used instead of le
size whenever feasible.
• Digital signature or publisher: Publishers are digitally signing their application les more frequently
than ever. A digital signature provides a reliable, unique value for an application le that is veried
by the recipient to ensure that the le is legitimate and has not been altered. Unfortunately, many
application les are not yet signed by their publishers, so using only publisher-provided digital
signatures as attributes is generally not feasible. Some application allowlists can be based on
verifying the publisher’s identity instead of verifying individual digital signatures. This assumes that
all applications from trusted publishers can themselves be trusted. This assumption may be faulty
if the software vendor has multiple applications, and your organization wants to restrict which of
those applications can be executed. Also, relying on the publisher’s veried identity might only allow
older software versions with known vulnerabilities to be executed. However, the benet of basing an
allowlist on publisher identities is that the allowlist only needs updates when there is a new publisher
(i.e., software vendor) or when a publisher updates its signature key.
• Cryptographic hash: A cryptographic hash provides a reliable, unique value for an application le, so
long as the cryptography being used is strong and the hash is already known to be associated with a
good le. Cryptographic hashes are accurate no matter where the le is placed, what it is named, or
how it is signed. However, a cryptographic hash is not helpful when a le is updated, such as when an
application is patched; the patched version will have a different hash. In these cases, the patch should
be identied as legitimate through its digital signature rst; then, its cryptographic hash should be
added to the allowlist. It is important to note that if the allowlist is not continuously updated with
new hashes for new and updated applications, there is a signicant risk of software not functioning
correctly. Further, if the allowlist is not continuously updated to remove existing hashes for older
software versions with known vulnerabilities, there is a signicant risk of vulnerable software being
allowed to run.
Choosing attributes is largely a matter of achieving the right balance of security, maintainability, and
usability. Simpler attributes such as le path, lename, and le size should not be used by themselves
unless there are strict access controls in place to tightly restrict le activity. Even then, there are often
signicant benets to pairing them with other attributes. A combination of digital signature/publisher
and cryptographic hash techniques generally provides the most accurate and comprehensive application
allowlisting capability, but usability and maintainability requirements can put signicant burdens on
your organization.
Application allowlisting is most often associated with monitoring executables. However, most application
allowlisting technologies can also monitor at least a few other types of application-related les, such as
libraries, scripts, macros, browser plug-ins (or add-ons or extensions), conguration les, and application-
related registry entries (on Windows hosts).”
41
41 Adam Sedgewick, Murugiah Souppaya, and Karen Scarfone, NIST Special Publication 800-167: Guide to Application
Whitelisting, National Institutes of Science and Technology (NIST) (October 2015), http://nvlpubs.nist.gov/nistpubs/
SpecialPublications/NIST.SP.800-167.pdf.

Cybersecurity Pracce #2: Endpoint Protecon Systems
33Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Initial implementation of application allowlisting may have major impacts to organizations as they try to
identify the multitude of executables used for approved applications. A clear plan should be created to
minimize operational impact. The plan should include:
• Audit mode: When deploying a solution, rst implement the software in audit mode. This will
provide a log of executables outside of the current approved list. Review the list to determine if any
executable should be added to the approved list.
• Enforcement mode: Once the solution has run for an appropriate time and the audit list has been
reviewed, update the solution to run in enforcement mode. This will begin to block the non-approved
executables from running.
• Support and tuning: After the solution has been implemented in enforcement mode, new applications
will be purchased and existing applications will be upgraded. Support and tuning needs to be
integrated into the application management lifecycle. Implement a plan to review new requests;
ensure this includes a process to review urgent requests, minimizing operational impact.
Organizations should maintain a current inventory of all software on endpoints to facilitate complete and
consistent maintenance and patching to protect against client-side attacks.
42
When examining solutions, organizations should consider choosing machine-level (PC/servers) or
network-level application allowlisting, or both. Conguration of application allowlisting is complex
and outside of the scope of this document. This activity should be done in conjunction with reviewing
administrative rights to endpoints.
2.L.E: Micro-Segmentation/Virtualization Strategies
NIST Framework Ref: PR.AC-5
Technologies called micro-virtualization or micro-segmentation assume that the endpoint will function in a
hostile environment. These technologies work by preventing malicious code from operating outside of
its own operating environment. The concept is that every task executed on an endpoint (e.g., click on a
URL, open a le) can run in its own sandboxed environment, thus prohibiting the task from interoperating
between multiple sandboxed environments.
Since most malware is installed by launching incremental processes after gaining an initial foothold, this
strategy can be effective at eliminating that second launch. Additionally, once the malicious task has
completed, the microenvironment is torn down and reset. Further conguration advice is specic to the
microenvironment technology deployed.
Key Mitigated Threats
1. Ransomware attacks
2. Loss or theft of equipment or data
42 “CIS Control 2: Inventory of Authorized and Unauthorized Software,” Center for Internet Security Controls (Accessed
September 24, 2018), https://www.cisecurity.org/controls/inventory-of-authorized-and-unauthorized-software/.

Cybersecurity Pracce #2: Endpoint Protecon Systems
34Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Suggested Metrics
• Percentage of endpoints encrypted based on a full eet of known assets, measured weekly. The rst goal
is to achieve a high percentage of encryption, over 99 percent. Achieving 100 percent encryption is
nearly impossible because process defects always exist. Additionally, the percentage of endpoints
encrypted will vary as you discover new assets, which is why it should be measured at least weekly.
• Percentage of endpoints that meet all patch requirements, measured monthly. The rst goal is to
achieve a high percentage of success. Secondary goals are to ensure that there are practices to patch
endpoints for third-party and OS-level application vulnerabilities, and to be able to determine the
effectiveness of those patches. Without this metric, there might not be checks and balances in place
to ensure satisfactory compliance with expectations. Rather than use the software distribution
technology for measurement, a secondary solution like a vulnerability scanner could be leveraged to
measure patch effectiveness.
• Percentage of endpoints with active threats, measured weekly. The goal is to ensure that practices are
in place to respond to AV alerts that are not automatically quarantined or protected. Such alerts
indicate that there could be active malicious action on an endpoint. An endpoint with an active threat
should be reimaged using genersal IT practices and managed using a ticketing system if forensics/
additional diligence is not required.
• Percentage of endpoints that run non-hardened images, measured monthly. The goal is to check assets
for compliance with the full set of IT management practices, identifying assets that do not comply.
To do this, place a key or token on the asset indicating that it is managed through a corporate image.
Separate practices are necessary for assets that are not managed this way to ensure that they are
properly hardened and patched.
• Number active endpoints with EOL issues or reaching EOL within the next 12 months. The goal is to bring
visibility to any ongoing or upcoming EOL concerns to assist in timely responses and resolutions. To
accomplish this, the asset management process is used to ag assets running EOL software and use
automated scans periodically to identify new or existing EOL. Separate practices are necessary for
assets that are not managed this way to ensure that they are properly decommissioned.
• Percentage of local user accounts with administrative access, measured weekly. The goal is to keep this
number as low as possible, granting exceptions only to local user accounts that require such access.
35Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #3:
Identy and Access Management
Areas of Impact
Passwords
Medium Sub-Practices
3.M.A Identity
3.M.B Provisioning, Transfers,
and Deprovisioning
Procedures
3.M.C Authentication
3.M.D Multi-Factor
Authentication for
Remote Access
Large Sub-Practices
3.L.A Federated Identity
Management
3.L.B Authorization
3.L.C Access Governance
3.L.D Single Sign-On
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
405(d) Resources
• Prescription Poster: Identity
and Access Management
Identity and access management (IAM) is a program that
encompasses the processes, people, technologies, and practices
relating to granting, revoking, and managing user access. Given the
complexities associated with healthcare environments, IAM models
are critical for limiting the security vulnerabilities that can expose
organizations. A common phrase used to describe these programs
is “enabling the right individuals to access the right resources at the
right time.”
Most access authentication methods rely on usernames and
passwords, a model proven to be weak by the success of phishing and
hacking attacks. Establishing IAM controls requires a distinct and
dedicated program to accommodate its high level of complexity and
numerous points of integration. You can nd a toolkit for establishing
an IAM program on the EDUCAUSE website.
43
This section will focus on the critical elements of an IAM program
required to manage threats relevant to the HPH sector.
Sub-Practices for Medium-
Sized Organizations
3.M.A: Identity
NIST Framework Ref: PR.AC-1
As dened in NIST Special Publication 800-63-3, “Digital identity is the unique representation of a subject
engaged in an online transaction.”
44
A common principle to follow is “one person, one identity, multiple
contexts.” In healthcare, a person can have the context of a patient, payor, or even employee of the health
system. For clinical staff, one person can have one identity, but that person’s ability to practice specialties
will depend on context. This includes the country, practice area, or hospitals where the person has a
business or employee relationship.
Within the United States, each worker is provided with a unique SSN. Similarly, a person who joins an
organization should be given a unique identier. That unique identier should not be used as a secret
authenticator, the way a person’s SSN is often used. The unique identier is not the authenticator.
43 Erik Decker, et al., “Toolkit for Developing and Identity and Access Management (IAM) Program,” EDUCAUSE (May 7,
2013), https://library.educause.edu/resources/2013/5/toolkit-for-developing-an-identity-and-access-management-
iam-program.
44 Paul A. Grassi, Michael E. Garcia, and James L. Fenton, NIST Special Publication 800-63: Digital Identity Guidelines, NIST
(June 2017), https://pages.nist.gov/800-63-3/sp800-63-3.html.
Cybersecurity Pracce #3: Identy and Access Management
36Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Establish each person’s identity through onboarding systems of record. The most common of these
systems is the ERP or HR system. When onboarding new employees in your organization, HR business
processes identify and establish the new employee in your organization. Onboarding involves many
processes, such as background checks, employment verication, and payroll preparation. They provide
solid identity proong used to verify the employee’s identity in the future. They trigger the generation of
the employee’s new digital identity. These identity-proong practices respond to the need to understand
a person’s relationship and context within your organization. Therefore, it is imperative that IAM
programs and functions align with HR practices and business processes. Identities maintain a series of
attributes that describe the common user elements. The series of attributes comes from the system
of record, whether that is an HR, contingent workforce, medical stafng ofce, or other system in your
organization’s ecosystem. Examples of common elements include a person’s name, location, telephone
number, email address, job title/job code, and specialization/practice data.
The system of record transmits attributes to the IAM system, enriching the identity data and facilitating
the ow of information to systems for login, access management, and other cybersecurity- and business-
related functions. In addition to common descriptive attributes, there may be other system-dened
attributes (e.g., roles or afliations used to describe populations of individuals: clinician, staff, staff
nurse, visitor, student). Organizations can leverage both types of attributes for future authorization
components. For example, you can use attributes to authorize eligibility for various systems (using a
technique called attribute-based access control [ABAC]).
Users dened under proper identity management processes will include more than your employees.
These processes should account for volunteers, locums, contractors, students, visiting scholars, visiting
nurses, physician groups staff, billing vendors, visiting residents, organ procurement organizations,
special statuses (such as emeritus professors), and third-party vendors that require access to provide
services to your organization. Each identity type must have an approved channel to serve as the system
of record, where the identity proong activities will occur. Care should be taken to manage non-
employees throughout their lifecycle since changes to their role and departure may not be as obvious
as it is for employees. Additionally, since a person can be an employee and non-employee (e.g., nursing
technician, nursing student, and volunteer) it is important to have the right contexts assigned to the
individual based on their roles. Ultimately, there should be an employed sponsor accountable for all
non-employee accounts.
This identity information can be stored in a single repository, enabling its consumption for other purposes.
IAM systems, in principle, are an aggregate of system of record data. IAM systems should be a system
of last resort when none exists (e.g., contingent workforce if HR/business does not have a solution). At a
minimum, follow these basic principles:
• Enumerate all authorized sources of identity. These sources are often referred to as the systems of
record. Examples include HR systems, vendor management systems, contingent workforce systems,
medical stafng ofces or practice ofces, and student information systems. Ensure that all users
receive a unique identity and identier. Smaller organizations without multiple constituents may
consider using the employee ID number from the system of record. Larger organizations with many
constituents should establish a unique identier for each user and reconcile. Do not use SSNs as
unique identiers. An individual with multiple contexts should have one user record with one unique
identier that ties to all contexts.

Cybersecurity Pracce #3: Identy and Access Management
37Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Maintain the integrity and uniqueness of digital identities. Never reuse identities for different people.
People come and go throughout the life of an organization. Maintain their records perpetually.
• Proper identity management enables the automation of functions such as system access and
authentication. Enumerate and establish attributes, which are critical to provide context to the
identity and required for access and authentication controls. For complex and large organizations,
this is an important principle to ensure the consistent application of attributes. For example,
it enables automated authentication and authorization through automated provisioning
and deprovisioning.
• Store identity information in a database or directory capable of registering identity information and
associated attributes. Such databases aggregate systems of record data. Consider specialized tools
for organizations with multiple constituent types.
• Use a single namespace to establish user accounts. Tie these user accounts back to the identity so that
you can always trace individuals to their digital identities.
3.M.B: Provisioning, Transfers and Deprovisioning Procedures
NIST Framework Ref: PR.AC-4
After you establish digital identities and user accounts, you must provision users with access to
information systems prior to using them. It is important to ensure that provisioning processes follow
organizational policies and principles, especially in the healthcare environment.
The HIPAA Privacy Rule’s minimum necessary standard requires organizations to implement procedures
that limit uses, disclosures, or requests of PHI to the minimum amount of data required to accomplish the
intended purpose. This same principle applies to reducing the attack surface of potentially compromised
user accounts. By limiting access, you can limit the scope of a ransomware outbreak or data attack.
Follow these principles for provisioning:
• Identify common systems that users need to access, and the least level of access required for each of those
systems. These common systems are referred to as birthright entitlements.
• Dene birthright entitlements in organizational policies, procedures, or standards. Documentation
should exist that describes the access rights that all users receive.
• Establish procedures and workows that ensure consistent provisioning of birthright entitlements.
Consider employing specialized tools to automate this process for accuracy and reliability. Do not
automate bad or unknown workows.
• Establish procedures and workows that enable provisioning of required access in addition to birthright
entitlements, such as access to auxiliary or ancillary systems. Pay special attention to cloud-based
systems. Consider leveraging federated access management tools that automatically provision
access in the cloud.
• Consider a two-part process that allows users to request access but requires a second individual to
approve the request prior to granting access. A common approach is to designate an employee’s
supervisor as the approving party. A secondary approval may be required for access to these
sensitive systems. The secondary approval can come from the executive owner of the data, or
their delegate.

Cybersecurity Pracce #3: Identy and Access Management
38Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Leverage IT ticketing systems by building the provisioning workow into the ticketing system. This
establishes consistency in the approval processes, automates the requesting and granting of approval, and
documents the granting of access. It is important to ensure access provisioning processes are auditable.
It is just as important to deprovision access in a timely manner as it is to enable the access when the users
request it. Unfortunately, unless deprovisioning processes are automated, it is likely that disabling access
might be missed, especially inside of a larger organization. As much as possible, it is recommended to tie
your key applications into a standard Single Sign-On platform, then deprovision access in an automated
manner once the termination request is conducted. This ensures that when the termination is processed
by HR, the user access will be promptly terminated. Follow these principles for deprovisioning:
• Establish procedures to terminate access to user accounts. Execute these procedures promptly at the
time of termination. Consider leveraging tools that automate this process after receiving notication
of termination from the system of record. The system of record is usually the HR system, although
other systems may trigger access termination.
• Ensure that your termination process, whether manual or automated, includes session termination steps
to prevent active sessions from remaining active. An example of this would be an email login on a
mobile phone remaining active after the employee leaves your organization.
• Establish an “urgent termination” process outside of the normal termination procedures. Use urgent
termination in cases of sensitive termination, such as an involuntary termination.
• Ensure that termination procedures include both critical business systems and ancillary or auxiliary
systems. Pay special attention to cloud-based systems that are accessible outside of your
organization’s standard network. These assets will remain accessible to the user if the deprovisioning
process is not completed, or if the system is not connected to an organization’s single sign-on
system. Consider using federated access management tools to deprovision access to cloud-based
systems automatically.
• Build automatic timeouts for nonuse in critical systems. These timeouts can catch edge cases
where deprovisioning procedures are not executed, ultimately reducing the exposure to
unauthorized access.
Removal of access should occur when users terminate their relationships with your organization and
when users transfer to new functions in your organization. For example, if a patient care services (PCS)
manager transfers to the nursing department, access granted when the user was a PCS manager should
be removed prior to granting access required by the user as a nurse. This helps to prevent users from
accumulating unnecessary access rights.
3.M.C: Authentication
NIST Framework Ref: PR.AC-7
User accounts must engage in authentication to properly assert the user’s identity in the digital
ecosystem. The most common and, unfortunately, weakest method for authentication relies on password
credentials. Nevertheless, password-based authentication systems will continue to exist for the
foreseeable future, and organizations should develop solid password authentication practices. Examples
of such practices are:

Cybersecurity Pracce #3: Identy and Access Management
39Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Centralized authentication: Use central authentication systems, such as Lightweight Directory
Access Protocol directories or Active Directory, to the greatest extent possible. Tying authentication
mechanisms back to these central systems enables enterprise management of credentials. You can
manage the access rights of your user base from a single location. This is incredibly important when
access needs to be deprovisioned in a timely and automated manner.
Passwords are the most common credential used to authenticate users. The strength and
management of passwords are paramount. Strong passwords combat brute force or password
guessing attacks. Assuming you can limit the exposure to brute force and guessing attacks, NIST
recommends the following techniques as part of NIST Special Publication 800-63:
45
¡ Limit the rate at which authentication attempts can occur. Spacing out each password attempt by a
second or two severely limits the ability of automated systems to brute force the password.
¡ Ensure the use of cryptographically strong hashing and salting for password storage.
¡ Use passphrases in place of passwords. Require a minimum of eight characters and permit up to 64
characters, as well all printable ASCII characters and spaces.
¡ Implement dictionary-based password checking and compromised password denylists. Prohibit
users from establishing risky passwords, such as those used in previous breaches, repetitive
or sequential characters, or context-specic words (such as a name of a service, username, or
derivatives thereof).
• Privileged account management: Centralized authentication should be used for both general
user access and privileged administrative accounts. Additionally, you should separate privileged
administrative accounts from general user accounts. For example, provision an IT administrator at
least two accounts: an account for use completing day-to-day activities and a separate administrative
account with access only to systems required by the IT administration function. This second step
is critical; the use of privileged accounts during normal day-to-day business may expose these
accounts to malware attacks, giving an attacker elevated access to your organization’s environment.
Limit this exposure as much as possible. Consider the following controls for managing your
privileged accounts:
¡ Ensure that the passwords set for service accounts are large and complex (at least 32 characters,
preferably 64).
¡ Rotate these passwords on a frequency you dene and require that the passwords are changed if
ever compromised.
¡ Escrow privileged systems credentials, making them unique for each system or device.
¡ Link privileged access to problem, change, or service tickets in your organization’s ticketing system.
• Require the use of a jump server when elevating privileges. Ensure full recording and auditing of the
jump server.
• Require brokered access to a privileged account. This should register which user is using the privileged
account and record all actions taken.
• Require MFA for all privileged accounts used interactively. Strong consideration should be made for the
use of hardware tokens, such as a Yubikey, when using MFA for privileged accounts.
45 Paul A. Grassi et al., NIST Special Publication 800-63B: Digital Identity Guidelines: Authentication and Lifecycle
Management, NIST (June 2017), https://pages.nist.gov/800-63-3/sp800-63b.html.
Cybersecurity Pracce #3: Identy and Access Management
40Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Conduct regular reviews of privileged access.
• Limit actions that privileged accounts can take by using access control lists. Check for the use of
sensitive commands and alert the IT or Cybersecurity departments if there is misuse.
• For further details on how to securely congure privileged access, consider the following resources:
¡ For Windows, see Microsoft’s article “Implementing Least-Privilege Administrative Models.”
46
¡ For Linux, see Redhat’s article “Controlling Root Access.”
47
• Local application authentication: There may be cases where applications do not support a centralized
authentication model. Although there are increasingly fewer onsite systems that cannot bind to
centralized authentication systems, these systems are still prevalent in the healthcare environment.
As organizations migrate applications to the cloud, it is easy to accidentally instantiate a cloud-based
service that lacks robust authentication and focuses on local user accounts.
Whenever you use systems with local authentication, you must maintain solid access control
procedures to manage user accounts. This requires designating a responsible IT owner who will
manage and regularly review these accounts. Failure to do this allows users access to systems
for longer than necessary and is especially risky when an employee leaves your organization and
continues to have access to these systems. Consider implementing these extra controls:
¡ Designate an IT owner for each legacy/cloud-based system.
¡ Establish a distribution list in your organization which includes your IT owners as members. Submit
terminations out to these IT owners as they occur.
¡ Ensure that IT owners comply with standard operating procedures for the onboarding, review and,
most importantly, termination of users.
¡ Regularly audit compliance with these manual processes. Ensure compliance with regular account
review and termination procedures.
¡ Monitor authentication attempts: Monitor both regular and privileged user accounts for security
and compliance purposes. Details are discussed further in Cybersecurity Practice #8: Security
Operations Center and Incident Response.
It is recommended to align authentication practices against NIST’s 800-63 Special Publication Series
(SP 800-63). Specically, within SP 800-63-B, three levels of authenticator assurances have been
established.
48
These levels can be applied based upon the sensitivity of the systems being accessed. The
higher the level of authentication assurance, the more sophisticated a bad actor will need to be to bypass
or circumvent these processes.
The 800-63B standard denes very specic authentication requirements. Below is a summary of these
for reference purposes. Detailed requirements should be referenced directly from NIST rather than
this publication.
46 Bill Mathers et al., “Implementing Least-Privilege Administrative Models,” Microsoft Windows IT Pro Center (Last
modied May 31, 2017), https://docs.microsoft.com/en-us/windows-server/identity/ad-ds/plan/security-best-
practices/implementing-least-privilege-administrative-models.
47 “Controlling Root Access,” Redhat Customer Portal (Accessed September 24, 2018), https://access.redhat.com/
documentation/en-us/red_hat_enterprise_linux/7/html/security_guide/sec-controlling_root_access.
48 Paul A. Grassi et al., NIST Special Publication 800-63B: Digital Identity Guidelines: Authentication and Lifecycle
Management, NIST (June 2017), https://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.800-63b.pdf.
Cybersecurity Pracce #3: Identy and Access Management
41Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Authenticator Assurance Level (AAL1): Single factor authentication
1. Types of authenticators: Username/Password, one-time password (OTP)
2. Reauthentication: Once every 30 days, regardless of user activity
3. Identity Proong: Meets low-impact systems dened in SP 800-53.
Authenticator Assurance Level 2 (AAL2): High condence of authentication requiring two different
authentication factors (multi-factor).
1. Types of authenticators: MFA (OTP, cryptographic), Username/Password + Single-Factor (OTP,
Cryptographic): If deployed via mobile phone the unlocking of a phone is NOT considered an
authentication factor.
2. Reauthentication: Once every 12 hours during extended sessions, once every 30 minutes for
inactivity. Can prompt user to cause activity prior to timeout.
3. Identity Proong: Meets moderate-impact systems dened in SP 800-53.
Authenticator Assurance Level 3 (AAL3): Very high condence of authentication through hardware-based
and cryptographic protocols.
1. Types of authenticators: Single-Factor Crypto HW + Username/Password, MFA OTP + Single-
Factor Crypto HW/SW, Single-Factor HW + MFA SW, Single-Factor HW + Single-Factor SW +
Username/Password.
2. Reauthentication: Once every 12 hours during extended sessions, once every 15 minutes for
inactivity. Can prompt user to cause activity prior to timeout.
3. Identity Proong: Meets high-impact systems dened in SP 800-53.
3.M.D: Multifactor Authentication
NIST Framework Ref: PR.AC-3, PR.AC-7
MFA systems require the use of several authentication methods to verify a user’s identity. According to
the common description, MFA systems use at least two of the following: something you know, something
you have, and something you are. Users must correctly address at least two of these three categories
before the system will verify their identities and allow access.
The most common MFA techniques use smartphone applications and deliver either push notications
to the phone or provide a one-time-code from the application that can be entered into the system being
authenticated to. Other examples include printing out one-time-codes ahead of time, use of hardware
tokens, or delivering one-time-codes through SMS messages. Another example is using biometrics
as a MFA technique. In all cases, the second factor is delivered to the user out-of-band from the
authentication technique. For example, most banks have MFA capabilities, which require the customer
to enter a password (something you know) followed by a verication code that is texted to the customer’s
smart phone (something you have).
MFA should be implemented on remote-access technologies to limit the value of password credentials
that could be compromised through phishing or malware attacks. MFA is an incredibly impactful method
for limiting an attacker’s ability to compromise your organization’s environment. Consider implementing
MFA on the following types of technologies:
Cybersecurity Pracce #3: Identy and Access Management
42Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• VPNs: These allow remote network access to your environment. VPNs should be congured to limit
user access based on role-based access control (RBAC) or ABAC rules and to enable MFA.
• Virtual desktop environments: These are environments where virtual terminal sessions can be
exposed to remote access, allowing your employees to work remotely. Although highly useful for
workforce exibility, virtual desktop environments systems can be compromised easily if they lack
MFA authentication.
• Email access: If your organization permits email access, MFA should be enabled to limit the risk of
compromised credential access in the email system. It is common for healthcare environments to
store PHI with these systems, and this exposure could result in a breach of sensitive information,
especially if MFA is not used. Take special precautions on the use of legacy email protocols, such as
IMAP and POP3, as these are not always compatible with MFA. For more details see Cybersecurity
Practice #1: Email Protection Systems.
One must also consider MFA techniques for hosted, or cloud-based systems. Internet accessible
applications (cloud or hosted on-premise) that allow access to sensitive information (e.g., payroll,
electronic medical records) should leverage MFA for authentication. To help organizations adopt MFA to
cloud based systems, tie MFA technologies into your single sign-on (SSO) platform. This way, any time you
deploy a new SSO implementation, you automatically get MFA added to it at no extra charge.
Sub-Practices for Large Organizations
3.L.A: Federated Identity Management
NIST Framework Ref: PR.AC-6
Federated identity management enables identity information to be shared between organizations
in a trusted manner. This allows identities from home institutions (e.g., individual clinics) to be used
across a greater ecosystem (e.g., the entire health network). In healthcare organizations, it is common
for providers, payors, and other afliates to work together in an integrated manner. In large complex
environments, multiple organizations operate jointly, with different HR practices inside each organization.
Rather than creating identities in each organization of a joint operation, federated identity management
tools and processes allow the identity assertions of the home institutions to be used throughout
the federation.
Consider the following example: a clinician is part of a practice group that is credentialed within a regional
hospital. From the hospital’s perspective, this clinician is not an employee but must be credentialed
with access to the electronic medical record (EMR). From the practice group’s perspective, this clinician
has been onboarded through standard HR background checks and processes. If the practice group and
the hospital were operating within a federation, the clinician’s “home” identity could be established
from the practice group and asserted to the hospital as part of the clearance processes. If the clinician’s
relationship with the practice group were to change, this identity information would be revoked within
the hospital based upon assertions from the federation. These processes would be completely automated.
The same model can be leveraged when working with third-party vendors that provide workforce support
or staff-augmentation capabilities. In this case, the third-party is the “home institution” that requires

Cybersecurity Pracce #3: Identy and Access Management
43Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
access to resources in your organization. To monitor the activities of each of those workforce members
would involve a highly complicated and largely manual process unlikely to be effective. A federation can
solve this problem.
In complex environments such as large integrated delivery networks, federations are almost a
requirement to properly manage the temporal aspects of the identities within.
3.L.B: Authorization
NIST Framework Ref: PR.AC-6, PR.AC-4
After authentication has occurred, the mechanism to obtain specic access to an information resource,
such as an application system, is referred to as authorization. Authorization processes check the level
of access that has been granted to a user credential and ensures that the credential can access only
preauthorized areas. Consider the analogy of traveling at the airport. When you pass through the
security lines, your identity is authenticated using your ID card or passport, and you are then authorized
to access the terminals based on a ticket for a ight. You are not permitted to access any other ight than
the one authorized on your ticket.
Access authorization controls support the HIPAA Privacy Rule’s minimum necessary standard to limit
the use, disclosure or request of PHI to the least amount of data to accomplish the intended purpose.
In addition to HIPAA compliance, minimum necessary is a leading practice to limit malicious use of
credentials. In most cases, when hackers break into systems, they are trying to access the “keys to the
kingdom” or privileged access credentials that permit access to the most sensitive resources. Do not risk
unauthorized access by granting more access than necessary to your users.
Consider adding the following controls to limit authorization to only those components required by
the user:
• Role-based access control (RBAC): Conduct a high-level role-mining exercise to map out the role
types that exist within your organization and the access they require. For example, identify access
requirements for clinicians, support staff, unit secretaries, switchboard operators, case managers,
and others. For example, the clinician may need access to the medical record (though not necessarily
the entire medical record), whereas the support staff may not need access at all. By dening the
unique requirements for these two roles, you have begun to differentiate access models. It can
be difcult to provision granular authorization models based on users’ roles. In healthcare, two
individuals might have the same job title and role, yet completely different tasks within your
organization. Relying solely on a person’s role to grant access could thus limit the ability for users to
fulll other authorized responsibilities.
• Attribute-based access control (ABAC): Attribute-based authentication models consider the attributes
associated with a user’s identity, the attributes of the information system being accessed, and the
context associated with the access request. In this model, a user may, for example, be granted an
attribute that enables the user to access a specialized function within an information system, but only
during business hours or only while onsite. When the user requests access, ABAC systems check the
actual context against the access requirements to determine whether access should be granted.
49
49 “Attribute Based Access Control,” NIST Computer Security Resource Center (Last updated February 13, 2013), https://
csrc.nist.gov/Projects/Attribute-Based-Access-Control.

Cybersecurity Pracce #3: Identy and Access Management
44Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
This highly effective model limits access based on user-specic rules established in the ABAC
systems that dene access parameters. As an example, a request is made to grant all nurses with
access to all patients on a specic oor in a specic hospital to support exible care requirements.
You might be concerned that this access is excessive because a nurse might not be part of a care
team for a particular patient. To reduce the risk to data, you can leverage ABAC, limiting access to
times when the nurse is physically present at a specic hospital and ensuring that access is granted
only after the nurse has been authenticated using both a password and MFA. The ABAC access
credentials cannot be used to grant remote access to the same patients or to grant access anywhere
else within the healthcare system. In this model, even a hacker with access to the password and the
MFA answer would be unable to access patients using those credentials.
3.L.C: Access Governance
NIST Framework Ref: PR.AC-4
When a user joins your organization, the onboarding processes generate a lot of access request activities.
Once access is established for a user, it can be a challenge to determine, at a given future time, whether
that access continues to be required. Consider an employee who has worked for your organization
for many years, serving in multiple capacities, and has been placed on special projects across your
organization. Over time, this employee might accumulate more access than was ever intended.
Conducting a manual review of each employee’s access to each of an organization’s critical application
systems would be nearly impossible. Fortunately, specialized tools are available that enable an
organization’s leadership to review system access in an automated, self-service capacity. These tools are
generally referred to as access governance tools. Below are the relevant components:
• Tooling: Specialized tools bind to identity management systems and connect to critical business
systems to understand the access in place for all users in these systems. These tools require the
ability to connect with and parse through specic aspects of the applications in question, such as
EMR systems, revenue cycle systems, imaging systems, lab systems, and more.
• Segregation of duties: Within access governance tools, specialized rules can be dened based on
roles or user attributes. For example, a nancial system must dene roles so that a clinician does not
have access to revenue cycle management functions. No employee should be capable of access with
both roles. Otherwise, a fraudulent purchase order could be generated, and the invoice paid by the
same person, resulting in a fraud loss to your organization. Understanding the characteristics and
requirements of these critical roles enables you to create automated alerts that control user access.
In addition to the standard segregation of duties checks, some specialized tools compare access
proles of certain users in a role to identify outliers. For example, these tools can assess the usual
pattern of access granted to nurses across multiple systems. This pattern can then be set as a
baseline of access, and the tool can compare each user against that baseline. If a specic nurse is
determined to have excessive access, the user can be reviewed for appropriate adjustments.
• Access review: Through workows established with these advanced tools, supervisors within your
organization can review the access that their employees currently have in critical environments. This
can be done on a regular schedule established by policy. In the case where an employee has retained
access that is no longer necessary, the manager can use self-service portals to identify these access
violations and ag them for removal. In automated systems, once a manager ags an access for

Cybersecurity Pracce #3: Identy and Access Management
45Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
removal, it be congured to be automatically stripped.
At the end of an access review, the manager can certify that the review is accurate. This
documentation is useful for audit practices and to demonstrate effective reviews.
3.L.D: Single Sign-On (SSO)
NIST Framework Ref: PR.AC-7
Federated Single Sign-On (SSO) is an effective method to authenticate users against centralized
credential repositories. SSO techniques abstract authentication principles away from the general
Microsoft- or Linux-based methods into a generalized standard that can be implemented across
platforms. SSO involves securely conducting a general authentication process and passing additional
identity attribute information to the specic authorization processes in the resources being accessed.
It also has the benet of requiring only one login while an active SSO session is enabled, eliminating
annoying password prompts.
Several federated SSO standards exist, including OpenID, Security Assertion Markup Language, OAuth,
and Active Directory Federation Services. When implementing cloud-based systems, such as software-
as-a-service (SaaS) systems, the use of SSO should be a security requirement.
A healthcare specic SSO model leverages a second authentication factor at clinical workstations for
easy access within a healthcare provider space. These systems can be congured to require a user to
authenticate once per day or per shift at a clinical workstation, after accessing the larger clinical setting,
using a password and key card/access badge. Subsequent authentications are conducted by tapping the
key card to provide secure, easy access to the clinical workstations. These systems provide MFA within
the clinical environment while easing the password authentication processes.
Key Mitigated Threats
1. Ransomware attacks
2. Insider, accidental or malicious data loss
3. Attacks against network connected medical devices that can affect patient safety
Suggested Metrics
• Number of alerts generated for excessive access to common systems, measured weekly. For example,
“allow any” permissions to core applications, SharePoint, le systems, etc.
• Number of users with privileged access, measured monthly. The primary goal is to establish a baseline of
the normal number of privileged accounts and monitor variances from the sbaseline.
• Number of automated terminations, measured weekly. The goal is to establish a baseline for normal
terminations and monitor variances from that baseline. A decrease in the number of terminations
can indicate that the automated systems are not terminating access properly.
• Number of elevated privileged access requests, measured weekly. The goal is to establish a baseline to
determine how much privileged access is granted over a one-week period and monitor variances
from that baseline.

46Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
All organizations within the HPH sector access, process, and transmit
sensitive information, including PHI or other personally identiable
information (PII). The data used in operations are highly sensitive,
representing a unique challenge to the HPH sector. It is common for
the healthcare workforce to leverage this type of data to carry out
their respective missions.
In that context, healthcare faces a growing challenge of
understanding where data assets exist, how they are used, and how
the data that is processed is transmitted. PII is exchanged, processed,
and transmitted between information systems daily. Protecting this
data requires robust policies, processes, and technologies.
51
As your organization substantiates its data protection and prevention
controls, it is best to begin by understanding the types of data that
exist in your organization, setting a classication schema for these
data, and then determining how the data are processed. Establish
a set of policies and procedures for normal data use and then
build in “guardrail” systems to guide your user base toward these
business processes.
Information can leak outside your network if you are not aware
of your network design, Healthcare Delivery Organizations (HDOs) networks consist of dozens of
traditional IT protocols (Server Message Block [SMB], Remote Authentication Dial-In User Service
[RADIUS], Universal Plug and Play [UPnP], Secure Shell [SSH], Remote Desktop Protocol [RDP], etc.) and
unique medical protocols (standard protocol such as Digital Imaging and Communications in Medicine
[DICOM], Health Level Seven [HL7], American Society for Testing and Materials [ASTM], Laboratory
Information Systems [LIS], Management Information Base [MIB] and several vendor proprietary
protocols). Organizations should monitor unencrypted trafc. With such a large and diverse network
to secure, aim for 360° top-down visibility to intelligently dene trust relationships between device
families, restrict lateral (in-group) communications, logically impose segmentation regimens outlined with
Cybersecurity Practice #6: Network Management, and easily maintain network architecture per best
practices. Trafc monitoring is needed to determine which devices are generating different type of trafc
and to establish a baseline for anomaly detection. For a visualization of this, see the PACS ecosystem
dataow visualization example.
Further details can be found in Cybersecurity Practice #5: IT Asset Management.
51 Erika McCallister, Tim Grance, and Karen Scarfone, NIST Special Publication 800-122: Guide to Protecting the
Condentiality of Personally Identiable Information (PII), (April 2010), https://nvlpubs.nist.gov/nistpubs/Legacy/SP/
nistspecialpublication800-122.pdf.
Areas of Impact
Passwords, PHI
Medium Sub-Practices
4.M.A Classication of Data
4.M.B Data Use Procedures
4.M.C Data Security
4.M.D Backup Strategies
4.M.E Data Loss Prevention
Large Sub-Practices
4.L.A Advanced Data Loss
Prevention
4.L.B Mapping of Data Flows
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
405(d) Resources
• Prescription Poster:
Data Protection and
Loss Prevention
Cybersecurity Pracce #4: Data
Protecon and Loss Prevenon
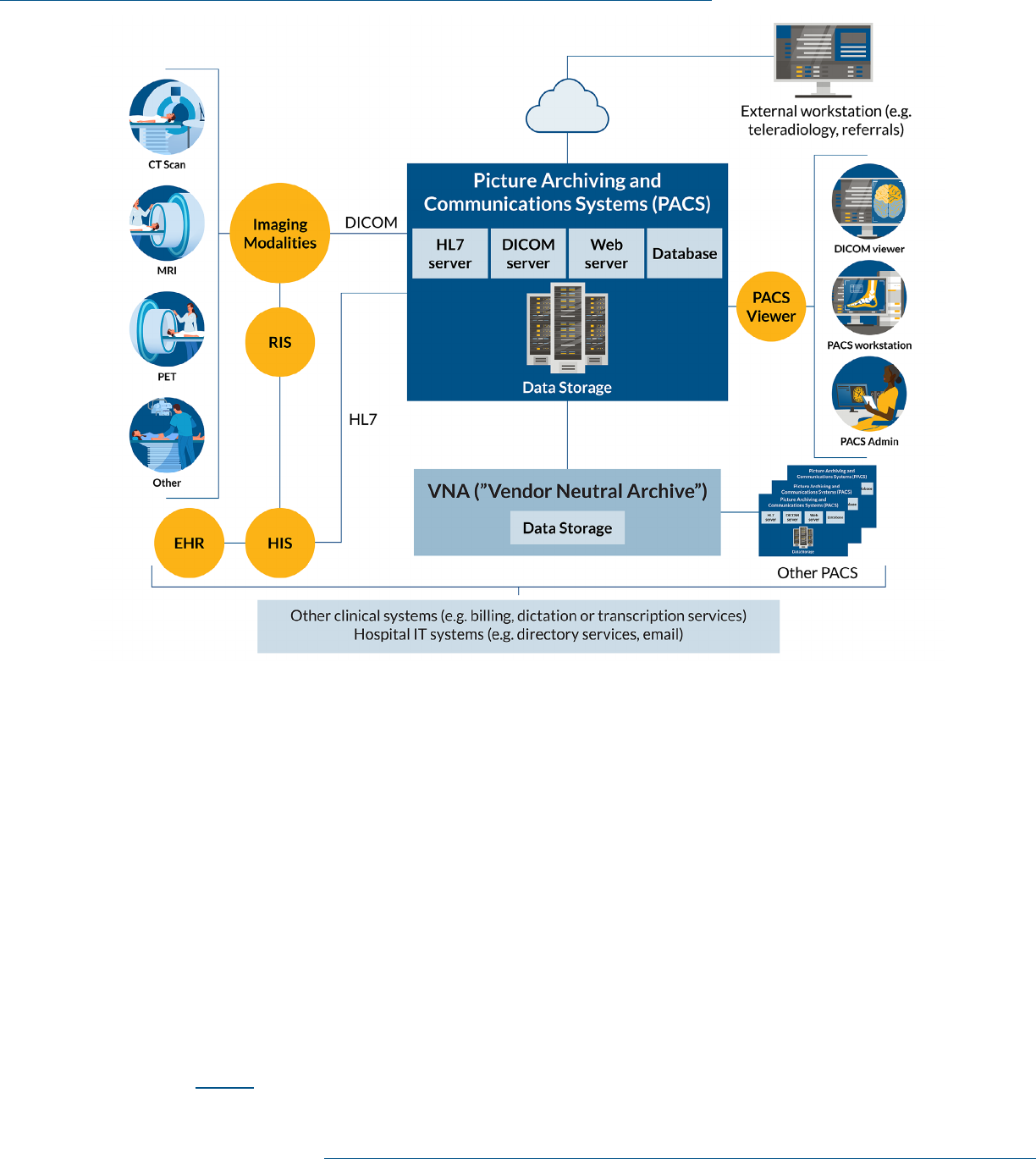
Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
47Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Medium-Sized Organizations
4.M.A: Classication of Data
NIST Framework Ref: (ID.AM-5)
There is a vast proliferation of data in healthcare environments. Data can range from PII (i.e., treatment
information, SSNs, insurance numbers, billing information) to research information. Data in healthcare
environments can also include business sensitive information such as strategies and development plans,
nancial data, HR information, and corporate board materials.
When determining data classications, consider not only condentiality but data integrity and availability
as well. For example, what if you can no longer trust the data is accurate because it has been damaged?
What if you can never have access to that data again because you can never retrieve or restore it?
Before establishing policies on how various data types should be used and disclosed, it is best to classify
them into high-level categories. This provides a consistent framework when developing policies and
procedures. Table 4 outlines a sample classication schema, with examples of the types of documents the
classication comprises.
Figure 1. PACS ecosystem dataow

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
48Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 4. Example of a Data Classication Schema
Classicaon Descripon Examples
Highly
Sensitive Data
Data that could easily be
used for nancial fraud
or could cause signicant
reputational damage.
SSN, credit card number, mental health information,
substance abuse information, infectious disease
treatment, employment/professional details, or other
demographic information.
Sensitive Data Regulated data, or
data that could cause
embarrassment to patients
or organizations.
Health information, clinical research data, insurance
information, human/employee data, and board materials.
Internal Data Data that are not
considered sensitive
but should not be
exposed publicly.
Policies and procedures, contracts, business plans,
corporate strategy and business development plans, and
internal business communications.
Public Data All data that have been
sanitized and approved for
distribution to the public
with no restrictions on use.
Materials published on websites, presentations, and
research publications.
4.M.B: Data Use Procedures
NIST Framework Ref: ID.GV-1
After data have been classied, procedures should be written on how to use these data based on
classication. These procedures describe the processes of setting usage expectations and of labeling the
information properly. These two functions are described further in the following paragraphs.
• Usage and disclosure: Based on the classication type, data use should be limited appropriately and
disclosed using specic methods. Consider the procedures in Table 4.
Be careful when sending information through email. Ensure that sending PHI via email is consistent
with the standards of the HIPAA Security Rule.
52
Do not send unencrypted PHI through regular email
or text message. Patients can request and receive access to their PHI via unencrypted electronic
communications following a brief warning that unencrypted communications could be accessed by
a third-party in transit. After reading this disclaimer, the patient must conrm that they still want to
receive the unencrypted communication.
• Labeling: It is important to label information properly to facilitate restriction implementation
related to its usage and disclosure. Labeling helps keep data secure in two ways. First, users will
understand how to handle information that is properly labeled. Second, specialized security tools,
such as data loss prevention (DLP) systems, can be congured to discover and control properly
labeled information.
52 “Does the Security Rule allow for sending electronic PHI (e-PHI) in an email over the Interent? If so, what protections
must be applied?,” HHS OCR (July 26, 2013), https://www.hhs.gov/hipaa/for-professionals/faq/2006/does-the-
security-rule-allow-for-sending-electronic-phi-in-an-email/index.html.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
49Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
At a minimum, the labeling process should ensure that labels are readily apparent when users view
information. Use techniques like placing the classication in the footer of the document. Collaborate
with your marketing and communication departments to create document templates based on data
classication levels. Organization-wide document templates allow specialized tokens or signatures
to be embedded in the documents and tracked by DLP systems.
Table 5. Suggested Procedures for Data Disclosure
Classicaon Use Disclosure
Highly
Sensitive
1. Must be restricted to the
minimum necessary for
individual job function.
2. Must use extreme caution when
handling data.
Only share information internally and only
when expressly permitted and when directed
by the data owner.
Sensitive
3. Must be restricted to the
minimum necessary for
individual job function.
Only share information internally and only
when expressly permitted.
Internal Use
4. Can be generally used, but
care should be considered in
its consumption.
Only share information internally within
your organization.
Public
5. No restrictions. Share freely with no restrictions.
4.M.C: Data Security
NIST Framework Ref: PR.DS, PR.DS-1, PR.DS-2, PR.IP-6, PR.DS-5
After policies and procedures have been dened, you can establish additional data security methods.
Consider the security methods described below in Table 6.
Table 6. Security Methods to Protect Data
Security Method Descripon Consideraons
Enable encryption Encrypt data in rest
and in transit
• When using the cloud-based services, enable native
encryption capabilities to prevent exposures if the cloud
provider is hacked.
• Ensure that full disk encryption is enabled on all
workstations and laptops.
• Encrypt highly sensitive data stored in lesystem or
within applications.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
50Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Security Method Descripon Consideraons
Encrypt data in
transit
Data retention
and destruction
• Ensure that websites containing sensitive data use
encrypted transport methods, such as Hypertext
Transfer Protocol Secure (HTTPS).
• Enable internal encryption methods when moving data in
your organization.
• Never send unencrypted sensitive data outside
your organization.
Data retention and
destruction
Contractually
bind third-parties
to destroy data
when terminating
contracts.
• Use standard destruction forms and require vendors
to attest that data have been destroyed pursuant to
those forms.
• Set retention policies and quotas on email systems to
reduce the amount of data that can be exposed. Ensure
that legal retention requirements are met.
• Establish a purge strategy that includes secure
deletion mechanisms.
Protect production
data
Scrub production
data from test
and development
environments
• Leverage specialized tools to deidentify data elements
within large systems (such as EMRs).
• Regularly audit data elements within test and production
environments to ensure that they are clean.
Protect sensitive
data
Mask sensitive data
within applications
• Permit SSN access only to members who require it (e.g.,
registration desks, admitting desks, payor processing).
4.M.D: Backup Strategies
NIST Framework Ref: PR.IP-4
A robust backup strategy for enterprise assets is critical to daily IT operations. It is equally important to
have a backup strategy in the event of cybersecurity incidents. There will be events that cause an asset,
or multiple assets, to be thoroughly compromised. During these events, routine backups can be the only
way to ensure proper execution of the recovery phase of your IR process. Fully decommissioning affected
assets and restoring them to a time before the compromise occurred is the best method to neutralize
the compromise.
At minimum, each mission-critical asset in your environment should have a backup plan. Backups can be
executed using a variety of methods, the most common being disk-to-tape, disk-to-disk, or disk-to-cloud
backups. The integrity of these backups is paramount; these copies are your last line of defense, and you
want to make sure they are complete and accurate when you need them.
No matter what backup strategy you choose, it is very important to make sure these backup locations are
not accessible from the general network or from general user populations. Backups may be the last line of
defense against a ransomware attack, so access to them should be severely limited.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
51Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
This includes access from the servers and systems themselves that are being backed up. Consider only
allowing systems to write new data rather than overwrite existing data. This can thwart the attempts of
encryption attacks against backup les.
Several commonly used backup strategies are listed below.
• Disk-to-tape: This method makes backups by accessing designated systems and les and writing all
content to a tape drive, or a tape library. Specialized software, hardware, and inventory controls are
required. To conduct backups efciently, you will need tape robots and a tape library appropriate
to the number and size of systems being backed up. These backups can be very large. Congure
the tapes to use a “write once and read many” option. It is of utmost importance that encryption is
enabled in writing to these tapes. If a tape is lost or stolen, unencrypted data could be breached.
There are great advantages to maintaining ofine backups. You can rely on these copies to be
available when you need them, and tape backups prevent attacks against the backup medium itself,
because they are ofine.
• Disk-to-disk: This method involves taking backup copies from a disk and replicating them to a
separate disk, or storage array dedicated to maintaining backup copies. This option generally costs
less than disk-to-tape strategies, and disk-to-disk backups usually execute more quickly than disk-
to-tape. It is important to use encryption on backup les in the event the les are copied outside of
your organization.
It is important to consider controlling access to the disk storage system as part of a disk-to-disk
approach. With cyber-attacks like ransomware, attackers intend to disrupt both production and
backup les. Attackers that launch ransomware attacks are aware that an organization’s rst
response will be to contain the ransomware and then restore the uncorrupted les from a backup
source. If they can compromise the backup and production les, it is more likely your organization
will pay a ransom to get its les back. Access control mechanisms should prevent the system being
backed up from accessing the disk array, except via required access channels. Do not permit other
access to the array from other accounts, including administrative accounts. Remember, everyone is a
potential target of a ransomware attack, especially administrators.
New “backup vaulting” tools can manage these access permissions and make it near impossible for
automated ransomware attacks to compromise the disk storage arrays. The use of these tools tends
to be expensive, so it is recommended to start with your mission critical applications and data rst, as
part of your Business Impact Analysis (BIA) processes.
• Disk-to-cloud: This method is very similar to disk-to-disk backup. Cloud backup offers multiple added
values, however. With a disk-to-cloud backup, you get the resiliency and exibility of the cloud
environment, as well as the benets from investments made by the cloud providers, to maintain 100
percent data availability. Rather than a single-point-of-failure model, as seen in disk-to-disk and
disk-to-tape backups, cloud providers replicate data backups, leveraging cloud infrastructure with
multi-fault–tolerant capabilities.
As with the disk-to-disk model, it is important to limit access to cloud-based backup storage to only
the systems and disks that are backed up and the data repository. Never implement a drive that
maps to the backup repository. That mapped drive could be the vehicle that delivers the ransomware
encryption. Always encrypt backup les to protect your organization if the cloud provider
is breached.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
52Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Disk-to-disk-to-cloud: This method combines the speed and local accessibility achieved with disk-to-
disk with the redundancy and off-site capabilities of the cloud. Information is backed up locally to
devices that meet the disk-to-disk requirements mentioned above. Those local devices then backup
to a cloud copy with archives.
When using cloud solutions, it is important to understand what your restore options are with
any selected solution. Ideally, if you must restore from the cloud copy of your data you want the
backup provider to ship you a disk with that data on it. Restores directly from the cloud can take an
exorbitant amount of time.
Two values every backup plan must include are the Recovery Time Objective (RTO) and Recovery Point
Objective (RPO). Your organization may have an affordable backup solution that you believe meets your
needs until you need to recover or restore data from the backup. One of the most crucial elements of a
backup plan is the plan’s restore capabilities, that is, to know how long it will take to do a complete restore
of the data and know what point in time your data will be at when the restore completes. A backup plan
alone is ineffective without the ability to restore the data.
Testing the restore is essential, as it determines if the backup contains the required information can be
restored at the point in time and within the timeframe you need. Without the objectives set (and a test to
prove the plan works) it is only a backup plan, not a restore plan.
Lastly, whatever method of backup is used, it is important to test the restoration of these backups on
a periodic basis to ensure data availability. Remember, your backup process is the last line of defense
and must be trustworthy in a time of need. Another consideration for selecting a backup method is the
amount of time it takes to restore data. Assessment of available methods should include disaster recovery
timing objectives.
4.M.E: Data Loss Prevention (DLP)
NIST Framework Ref: PR.DS-5
Once standard data policies and procedures are established and the workforce is trained to use them, DLP
systems should be implemented to ensure that sensitive data are used in compliance with these policies.
Multiple DLP solutions exist and can be applicable depending on the types of data access channels that
need to be monitored. Traditionally, DLP systems monitor email, le storage, endpoint usage, web usage,
and network transmission. All these channels should be considered.
A challenge with DLP systems is to determine which methods will be used to positively identify sensitive
information. Within a healthcare environment, that can be tricky. Generally, there are two approaches,
both have limitations:
• Identify sensitive data based on dictionary words that may trigger the inclusion of sensitive data. These
dictionaries include robust language repositories that identify health information. The challenge
with this technique is terminology. Medical terms are often used in the regular course of business,
outside the context of sensitive information. This can lead to a high rate of false positives, forcing the
workforce to apply prevention practices that are not necessary.
• Identify sensitive data based on identiers that are known to be sensitive, a process known as matching.
There are two popular methods of matching: (a) leveraging tokens embedded in documents classied
as sensitive (document matching) and (b) leveraging actual patient identiers from your EMR (exact

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
53Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
data matching). Document matching dramatically reduces the number of false positives. However,
the workforce must be trained on proper data classication. With exact data matching, the false
positive rate will be lower than with the dictionary approach since it involves positive conrmation.
Exact data matching requires regularly extracting information from the EMR to load these identiers
into the system. Extra precautions must be taken so that the resulting large datasets are not exposed.
Once your identication methodology is established, DLP systems can be congured to monitor data
access channels of interest and make policy decisions based on the data types and the access channels.
It is best to provide direct feedback to users when the data policy has been violated, to avoid recurrent
violations. Real-time feedback helps users adjust their data usage behaviors effectively. Data channels
are presented in Table 7 for your consideration.
Keep in mind DLP technology does not have perfect visibility and matching. If data is encrypted, DLP may
not have visibility to the contents. In addition, DLP may not have visibility to all communication channels
(e.g., SFTP, SCP). For a determined insider, DLP may not prevent theft of data captured through cameras,
copy/paste, printing, etc.
Table 7. Data Channels for Enforcing Data Policies
Data Channel Implementaon
Specicaon
Consideraons
Email Implement inline through
Simple Mail Transfer
Protocol (SMTP) routing
for email messages
delivered outside
your organization.
• Dene thresholds of risky behavior. Implement a
DLP block for these thresholds (e.g., > 100 records of
PHI in the email).
• Dene thresholds of risky behavior. Implement a
DLP encrypt action for these thresholds, forcing the
message to be encrypted before delivered.
Endpoint Install DLP agents on
managed endpoints that
can apply data policies.
• Standardize and deploy encrypted thumb drives to
users who require mobile storage options.
• Prevent the copying of data to unencrypted thumb
drives, or force encryption when copying data.
• Control the use of noncontrolled peripherals and/or
storage devices (e.g., backups of iPhones on devices).
Permit only when specically authorized.
• Conduct data discovery scans of data residing on
endpoints, exposing data on the endpoint so the user
can make data destruction decisions.
Network Implement through
Switched Port Analyzer
(SPAN) ports from egress
network points or through
internet Security Content
Application Protocol
(SCAP) on web proxies.
• If online, prevent the leakage of unencrypted
sensitive data based upon predened thresholds
(e.g., les that contain > 100 records of PHI).
• If out of band, activate IR procedures to contain data
leakages that occur through the network.
Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
54Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Large Organizations
4.L.A: Advanced Data Loss Prevention
NIST Framework Ref: PR.DS-5
After implementing basic DLP controls, consider expanding your DLP capabilities to monitor other
common data access channels. Table 8 below includes recommended methods for this.
Table 8. Expanding DLP to Other Data Channels
Data Channel Implementaon
Specicaon
Consideraons
Cloud storage Use cloud access
security broker
(CASB) systems
to monitor
data ows into
cloud systems.
• Label data identied as sensitive. Implement digital rights and
encryption to limit access to sensitive data.
• Ensure that cloud-based le storage and sharing systems do not
expose sensitive data in an “open sharing” construct without
authentication (i.e., do not permit the use of sharing data
through a simple URL link).
• Establish technical cloud-based security policies matching your
organizational security policies.
Onsite le
storage
Point discovery
scanning systems
at known le
servers or other
large data
repositories.
• Conduct regular DLP scans against the le systems to scan and
identify sensitive data.
• Query security access permissions for each le containing
sensitive data. Dene thresholds for excessive access and
set alerts if these are crossed. Forward alerts to the SOC for
response, as described in Cybersecurity Practice #8: Security
Operations Center and Incident Response.
• Determine relevance and age of records with sensitive data.
Consider executing data destruction practices for records that
have not been opened or viewed for an extended duration.
• Determine data ownership of sensitive les identied in
le storage systems, leveraging automated tools. Establish
workow options allowing data owners to provide input into
access permission reviews of their sensitive les.
Web-based
scanning
Congure DLP
systems to crawl
known public
websites for
sensitive
information.
• Conduct a “spearing” exercise, which is like methods deployed
by search engines. Compare les and results posted on websites
against DLP matching policies and respond quickly to any
sensitive data that are exposed.
• Conduct manual searching activities on a periodic basis over
exposed websites. Look for les that may contain large amounts
of sensitive data (e.g., xls(x), csv, txt and pdf).
Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
55Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
4.L.B: Mapping Data Flows
NIST Framework Ref: ID.AM-3, DE.AE-1
The process of mapping data ow requires evaluating each application used and the information that
ows throughout your organization. This process is broader than IT, so all data stakeholders must
be engaged. The data mapping process should include both vended as well as internally developed
applications. For internally developed applications, you may be able to partner with stakeholders in your
organization’s software development lifecycle process. For vended applications, you may be able to
partner with stakeholders in your organization’s supply chain process.
In 2019 the Healthcare and Public Health Sector Coordinating Council (HSCC) released a new
publication, the Health Industry Cybersecurity Supply Chain Risk Management Guide (HIC-SCRiM).
53
This publication describes processes and techniques for managing all third-party risk. It also includes
sample questionnaires for vendors to complete, which can be used to gather information for mapping data
ows. These same questions can be asked of internal development teams.
The process also requires an understanding of all the applications used, as well as the information
they contain and exchange with other applications. Data mapping documentation should be reviewed
periodically to reect changes in your organization’s data needs. Leverage contract initiation or renewal
events as ideal times to review non- or pre-existing data mapping documentation.
By following this process and maintaining an accurate mapping of data ow, an organization can quickly
adapt to application system changes, such as upgrades, patches, integrations, and migrations. The
mapping process also ensures protection of data integrity through the understanding of “what data
lives where.”
After data business practices are dened, it is advisable to outline these processes in a data map. Data
maps should include the following components:
• Applications that house sensitive data
• Standard direction movement of data
• Users of applications and data
• Methods used to store and transmit data
Data mapping documentation does not need to be visually formatted, although data ow diagrams can be
very useful. The data mapping documentation should provide enough information to answer some basic
questions about the data itself:
• Where does the data come from?
• Who can access the data and how do they do it?
• How are users authenticated?
• Once authenticated, what data can users access?
• Where is the data stored?
• What can users do with the data?
• Where is the data retained, and for how long?
53 Health Industry Cybersecurity Supply Chain Risk Management Guide v2.0, Healthcare and Public Health Sector
Coordinating Council (HSCC) (September 2020), https://healthsectorcouncil.org/hic-scrim-v2/.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
56Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Conducting this type of mapping, and potentially adding it to a larger enterprise architecture reference,
enables an organization to identify data protection and monitoring requirements. Data mapping often
results in more concrete information about the data managed by the enterprise, due to the ability to track
attributes such as:
• Data ownership (business and technical owners)
• Data classication (public, private/internal, sensitive/regulated, etc.)
• Data type (PHI, PII, PCI, etc.)
• Data elements (patient name, MRN, DOB, etc.)
• Data location (data center, cloud, mobile device, etc.)
• Number of records stored
• Number of records processed, annually
• Number of users
Data mapping exercises can be a daunting task. It is important to understand that this may take time and
effort to fully implement. It is recommended that a data mapping plan be created to ensure success. The
plan should include:
• Start with one set of data at a time. Focus on one set of data at a time. For example, start with PCI
information and then move to PHI, etc.
• Inventory of location. Once you understand the category of data, create an inventory of where the
data is located. This can be done through surveys or interviews of application and database owners.
• Source categories and data collection. Once you know the location, develop categories of where the
data comes from and how the data is collected.
• Access rights. Once you know the location and the data collection source, understand how access is
granted to the data. This should include an understanding of the various business roles with access
to the data.
• Data ow. Once the location is understood and the source of the data, appropriate data ow
diagrams can be created to understand the data in transit (as it is forwarded in and outside
your organization).
If your organization is new to the process of mapping data ows, various tools and examples can be
found online.
Finally, note that not all data managed or owned by your organization will be contained or used in
applications. In addition to internally developed and vended applications, consider data exchanges/
interfaces (SFTP, HL7, FHIR, etc.), research projects, cloud APIs, medical devices, networking devices,
mobile devices, etc. as potential data mapping subjects.
Key Mitigated Threats
1. Ransomware attacks
2. Insider, accidental or malicious data loss
3. Loss or theft of equipment or data

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
57Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Suggested Metrics
• Number of encrypted email messages, measured weekly. The goal is to establish a baseline of encrypted
messages sent. Be on the lookout for spikes of encryption (which could indicate data exltration) and
no encryption (which could indicate that encryption is not working properly).
• Number of blocked unencrypted email messages with sensitive data, measured weekly. The goal is to
detect large numbers of blocked messages, which could indicate potential malicious data exltration
or user training.
• Number of les with excessive access on the le systems, measured weekly. The goal is to enact
actions that limit access on the le storage systems to sensitive data, create tickets, and deliver to
access management.
• Number of unencrypted removable devices with access attempts, measured weekly. The goal is to use
this information to educate the workforce on the risks of removable media.
• Number or names of applications in high-risk categories. The goal is to identify and prioritize
applications to protect. Applications that manage many sensitive, regulated, or protected data
records with many users may be candidates for higher levels of protection than applications that
manage fewer records, don’t manage sensitive, regulated, or protected data, and have few users.
• Percentage of applications with complete data mapping documentation. The goal is to measure how
much of your organization’s data is documented and ultimately, appropriately protected.
• Number or percentage of applications with refreshed data maps that comply with the refresh policy.
The goal is to ensure that data mapping documentation does not become stale and is refreshed at
appropriate timeframes.

58Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #5:
IT Asset Management
Areas of Impact
PHI
Medium Sub-Practices
5.M.A Inventory of Endpoints
and Servers
5.M.B Procurement
5.M.C Secure Storage for
Inactive Devices
5.M.D Decommissioning Assets
Large Sub-Practices
5.L.A Automated Discovery
and Maintenance
5.L.B Integration with Network
Access Control
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
• Attacks against network
connected medical
devices that may affect
patient safety
405(d) Resources
• Prescription Poster: IT
Asset Management
The process by which organizations manage IT assets is generally
referred to as IT asset management (ITAM). ITAM is critical to
ensuring proper cyber hygiene controls are in place across all assets
in your organization. ITAM increases the visibility of cybersecurity
professionals in your organization and the use of discovery tools
reduces unknowns.
ITAM processes should be implemented for endpoints, servers,
application, and networking equipment. The cybersecurity practices
in this section assist and support every other cybersecurity practice
identied in this publication. ITAM cybersecurity practices can be
difcult to implement and sustain, but they should be incorporated
into every lifecycle stage of IT operations to maintain data accuracy
and integrity. For each asset, the lifecycle includes procurement,
deployment, maintenance, and decommissioning. Though each type
of asset is used differently during its lifecycle, the lifecycle itself
is consistent. As part of its public–private partnership with the
NIST National Cybersecurity Center of Excellence (NCCOE), the
nancial sector has written a detailed ITAM practice guide: IT Asset
Management.
54
Though written for a nancial-sector audience, the
methods discussed in the guide are easily applied to the HPH sector.
Sub-Practices for Medium-
Sized Organizations
5.M.A: Inventory of Endpoints and Servers
NIST Framework Ref: ID.AM-1
The rst ITAM component that should be implemented is an inventory archive buildout. This critical
technology component provides a normalized, consistent approach for organizations to store
inventory data.
Important data elements and attributes should be captured for each asset in the ITAM. It is recommended
to evaluate following granular device attributes for inclusion in your ITAM:
• AssetID (primary key)
• Hostname
• Operating System—Type, version, patch level, hostname
54 Michael Stone et al., NIST Special Publication 1800-5b: IT Asset Management, NIST(October 2015), https://nccoe.nist.
gov/sites/default/les/library/sp1800/fs-itam-nist-sp1800-5b-draft.pdf.

Cybersecurity Pracce #5: IT Asset Management
59Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Media Access Control (MAC) Address
• Internet Protocol (IP) Address
• Deployed to (User)—Users associated with current of past login or sessions
• Last Logged on User
• Purchase Date
• Device Category
• Manufacturer and model
• Firmware—Type and version
• Software Prole—Installed applications version, open ports
• External components—DOK, Portable Hark Disk, etc.
• Network Context—MAC, IP, VLAN, Connection Type, Access Point/Switch, SSID, managed/
unmanaged device, open ports, inbound/outbound trafc
• Organizational Context—Location, site, organizational unit
• Unique Tags—Serial number, Recall needed, MDS2, Lost, New, Device ownership (company managed
device, employee’s personal device, vendor’s device etc.)
• Data Type—PHI (storing/transmitting), PCI
A robust ITAM repository becomes your single source of truth for all IT assets in your organization. This
repository will be maintained and trusted to be highly accurate and actionable.
Special consideration should be given to the differences between ITAM systems and device management
systems. Device management systems, which connect to IT devices like endpoints and servers, can
automate the management and maintenance of these assets. They are highly effective at executing
tasks such as software discovery, patch management, and performance monitoring. However, device
management systems cannot account for the addition and removal of IT assets or answer the inevitable
question, “Where did that laptop go?” They manage an organization’s devices at a single point in time and
are not workow driven.
IT service management tools (e.g., ticketing systems) can be integrated with IT general controls to ensure
accurate and precise asset management through standard performance management activities.
55
55 “CIS Control 1: Inventory and Control of Hardware Assets,” Center for Information Security Controls (Accessed
September 24, 2018), https://www.cisecurity.org/controls/inventory-and-control-of-hardware-assets/.

Cybersecurity Pracce #5: IT Asset Management
60Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
5.M.B: Procurement
NIST Framework Ref: ID.AM
A critical milestone for success is to incorporate the ITAM processes into the supply chain program.
The goal is to have supply chain activity from across your organization proactively entered in the ITAM
system. The result will be that each technology asset, endpoint, server, or networking equipment is
registered in the ITAM system as it is acquired.
An example of integration of the ITAM process into your organization’s existing supply chain scheme is to
introduce a process. This process should include the following steps:
• Step 1: Identify each department that can procure or acquire technology.
• Step 2: Work with the supply chain departments and establish a centralized workow (such as a
ticketing system) for the ordering of technology. This could be considered the rst step in the asset’s
lifecycle tracking.
• Step 3: As part of the workow, inform the IT department of the new technology being ordered. This
can be accomplished through a ticket that assigns a specic task to the IT department for setting up
the asset.
• Step 4: Receive the asset from the supplier. As part of the receiving of the asset, update the workow
(or ticket) and collect the asset information previously referenced in section 5.M.A: Inventory of
Endpoints and Servers. Data about the new asset can be captured physically, at a shipping dock, or
virtually for virtual technology purchases.
Some organizations may choose to adopt an advanced approach where the procurement process
may be automated to capture characteristics or attributes details of new assets. Automation of the
process reduces the manual labor required and the exposure to human error in collecting the data.
• Step 5: As an asset is acquired, it must be tagged it with an asset tag. These tags can be physical
or logical. The tagging process ensures that the asset has a unique ID that can be used to identify
it in the ITAM system. Assigning a unique ID that uses existing attributes of the technology (e.g.,
hostname, IP address, MAC address) is not recommended. These elds aligned with these attributes
may change, potentially creating duplicate records.
5.M.C: Secure Storage for Inactive Devices
NIST Framework Ref: PR.AC-2
Assets that are not in circulation should be returned to the appropriate IT department for secure storage.
Storage areas (e.g., lockers, cages, rooms) should be secured with physical access controls. Access should
be limited to those who require it. As assets are being stored they should either be securely wiped or
full-disk encryption should be veried. In both cases, it is important to have these records in place in the
event the device is misappropriated, and a forensic analysis of data exposure is necessary. Physical access
controls may include badge readers, video camera surveillance, and door alarms.
If an asset is identied for redeployment, it should be securely imaged to deploy a “fresh” computer
system for the new user. This ensures that old sensitive data are removed and that the asset has a clean
bill of health.

Cybersecurity Pracce #5: IT Asset Management
61Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
When an asset is sent to storage for redeployment or processing, the ITAM system should be updated
to reect a change of ownership and new physical location (i.e., storage) for the asset. If the asset is
redeployed or decommissioned, the ITAM system should be updated again to reect its new status.
5.M.D: Decommissioning Assets
NIST Framework Ref: PR.IP-6, PR.DS-3
It is critical to properly dispose of retired assets, as they may contain sensitive information. When
executing destruction and certication procedures, update the ITAM to indicate that the device has been
decommissioned. This establishes a permanent record in your asset management source of truth, the
ITAM. The following procedures should be completed when decommissioning an IT asset:
• Central collection: IT assets should be collected and stored in centralized, physically locked areas
prior to decommissioning. Your workforce must be trained to turn in any asset that they no
longer use.
• Central destruction/wipe: Assets that are collected for decommissioning must undergo a secure
process to destroy or electronically wipe the storage media. This ensures devices are properly
sanitized before leaving your organization’s possession for destruction. Permanent removal of
storage media may be completed by your IT organization or an external service provider. It is a good
practice to obtain and archive a certicate of destruction for audit purposes.
• Record keeping: Once the IT asset has been cleared for removal from your organization, the asset
ITAM record should be registered for destruction or decommissioning. Certicates of destruction
can be stored in the ITAM record for easy access. It is highly advisable to not delete the asset record.
Instead, update the asset’s status in the ITAM system to reect it has been decommissioned and is no
longer owned by your organization. You may need to refer to the asset record in the future.
Sub-Practices for Large Organizations
5.L.A: Automated Discovery and Maintenance
NIST Framework Ref: PR.MA-1, PR.MA-2, PR.DS-3
Once your ITAM system is in place and your procurement processes are registered, the challenge is
maintaining the records. Large organizations can have tens of thousands of endpoints and thousands
of servers. As attributes must be kept for each asset, it can mean hundreds of thousands to millions of
unique data elements require management across the entire ITAM system.
It is very difcult to manually maintain hundreds of thousands of data elements. After an asset is
acquired, without the exercise of proper asset management controls, it could be deployed sometime in
its lifecycle in unforeseen ways. For example, a new laptop may be issued to a user. That user may leave
your organization, turning in the laptop to a supervisor. The supervisor may assign the laptop to the new
employee who lls the open position. Unless IT is informed and the ITAM is updated, the asset record for
the laptop (now assigned to a different user) will be wrong.

Cybersecurity Pracce #5: IT Asset Management
62Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Another common example relates to an existing asset’s upgrade or hardware change to an existing asset.
This asset might change operating system or patch levels. Maintaining that information manually in the
ITAM is nearly impossible.
Automated discovery systems can maintain these records and account for both scenarios described
above. In the case where an asset changes hands to a new user, discovery tools can register login
occurrences for the “assigned user” and for the “actual logged in user.” If a threshold is triggered
(indicating that the assigned user no longer logs in and a different user continually logs in), a change-
in-ownership process can be triggered. This process may be automated, requiring no intervention, or
manually completed by generating a ticket to validate the change of ownership. In the case of operating
systems patching levels, automated discovery systems can provide snapshot views of current patching
levels for assets. When these snapshots are compared by cybersecurity vulnerability management
systems, vulnerabilities due to obsolete software versions will be identied across the eet.
5.L.B: Integration with Network Access Control
NIST Framework Ref: PR.AC-4, PR.AC-5, PR.AC-6
The practices outlined so far assume normal acquisitions processes. However, there are times when IT
assets are integrated in your organization by means other than standard supply chain channels. Examples
include personal devices (i.e., BYOD) and assets that are donated or provided free-of-charge as part of a
third-party contract.
Without oversight, it is difcult to detect and track these assets. Outliers can be controlled by integrating
your NAC and ITAM systems. Further details can be found in Cybersecurity Practice #6: Network
Management. It is also difcult, and time consuming to track and protect the ow of data through these
assets. Further details can be found in Cybersecurity Practice #4: Data Protection and Loss Prevention.
Key Mitigated Threats
• Ransomware attacks
• Loss or theft of equipment or data
• Insider, accidental or malicious data loss
• Attacks against network connected medical devices that may affect patient safety
Suggested Metrics
• Percentage of devices added to ITAM system through procurement channels, measured monthly. The goal
is to establish a baseline and achieve a higher percentage over time.
• Number of devices added to the ITAM from NAC systems, measured weekly. The goal is to analyze spikes
after initial deployment, which may indicate a problem capturing or maintaining asset records.
• Number of devices properly removed from asset management system using proper decommissioning
channels, measured weekly. The goal is to ensure devices are properly decommissioned. Lack of
execution of these processes over a period may indicate a compliance issue.
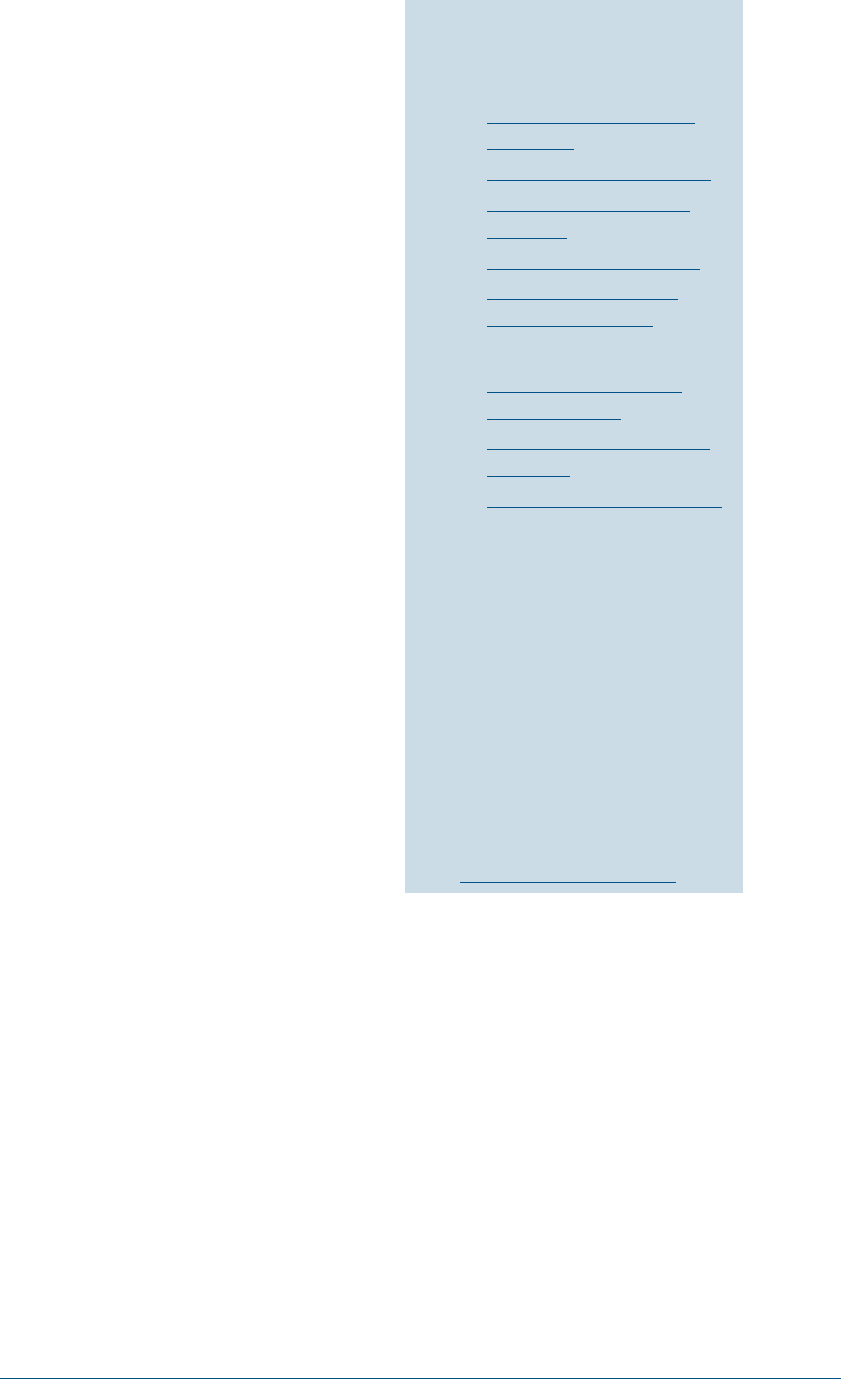
63Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #6:
Network Management
Areas of Impact
PHI
Medium Sub-Practices
6.M.A Network Proles and
Firewalls
6.M.B Network Segmentation
6.M.C Intrusion Prevention
Systems
6.M.D Web Proxy Protection
6.M.E Physical Security of
Network Devices
Large Sub-Practices
6.L.A Additional Network
Segmentation
6.L.B Network Analytics and
Blocking
6.L.C Network Access Control
Key Threats Addressed
• Ransomware attacks
• Loss or theft of equipment
or data
• Insider, accidental or
malicious data loss
• Attacks against medical
devices that can affect
patient safety
405(d) Resources
• Prescription Poster:
Network Management
Organizations leverage IT networks as a core infrastructure to
conduct business operations. Without networks, there would be
no interoperability. Networks must be deployed securely to limit
exposure to the potential impacts of cyber-attacks. Network design
will have a direct impact on how well you can thwart some of the
more nefarious cyber-attacks, such as ransomware attacks. Network
diagrams are crucial to network management. They can:
• Provide visibility to current network segmentation, including
analysis of each device type (medical and non-medical devices) in
each segment, connectivity between VLANs, and breakdown of
devices by type and vendor.
• Be designed to associate a risk level for each segment/VLAN.
• Demonstrate highly granular visibility to achieve more precise
baselining and greater context awareness.
• Allow for more accurate device classications, delivering
greater functionality and safe use insights (with which to dene
trust relationships).
• Represent a real-time viewpoint into inter-device trafc ows to
inform attack detection and access policies.
Sub-Practices for Medium-
Sized Organizations
6.M.A: Network Proles and Firewalls
NIST Framework Ref: PR.AC-5, PR.AC-6
An effective network management strategy includes the deployment of rewalls to enable proper access
inside and outside of your organization. Firewall technology is far more advanced than standard router-
based access lists and is a critical component of modern network management. Organizations should
deploy rewall capabilities in the following areas: on wide area network (WAN) pipes to the internet
and perimeter, across data centers, in building distribution switches, in front of partner WAN/VPN
connections, and over wireless networks.
There should be clear boundaries that determine how trafc is permitted to move throughout
your organization, including a default-deny ruleset whenever possible. At the perimeter, inbound
and outbound rules must be congured with a default-deny ruleset to limit accidental network
exposures. This often complicated process can be achieved by establishing security zones through
network segmentation.

Cybersecurity Pracce #6: Network Management
64Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Consider limiting the outbound connections permitted by assets in your organization. This can be a
challenge to implement organization-wide. However, for zones of high sensitivity, egress limiting can
prevent malicious callbacks or data exltration. The SOC should monitor egress logs, as outlined within
Cybersecurity Practice #8: Security Operations Center and Incident Response.
Firewall rules may change when technology is added or removed. A robust change management process
should include reviewing every rewall to identify necessary changes. These change requests should
comply with standard IT operations change management processes and be approved by cybersecurity
departments before any rewall is modied. Refer to sub-practice 7.M.E: Change Management for more
details on change management.
As part of standard rule management for rewalls, it is important to periodically review rewalls to ensure
they are properly structured as required by cybersecurity teams. Consider implementing a monthly or
quarterly review of the highest-risk rulesets.
6.M.B: Network Segmentation
NIST Framework Ref: PR.AC-5
Partitioning networks into security zones is a fundamental method of limiting cyber-attacks. These zones
can be based on sensitivity of assets within the network (e.g., clinical workstations, general user access,
guest networks, medical device networks, building management systems, IoT networks) or standard
perimeter segmentations (e.g., DMZ, middleware, application servers, database servers, vendor systems).
Examples of standard network zones are as follows:
Figure 2. Firewall Segmentation

Cybersecurity Pracce #6: Network Management
65Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Perimeter defenses: Most organizations host services that are accessed through the internet. A
robust defense strategy should be deployed to monitor these “front doors.”
56
Best practices for perimeter defenses include the following:
¡ Implement highly restrictive rules on inbound and outbound ports and protocols. Use default-deny
rules in rewalls and enable access only when clearly understood.
¡ Restrict DMZ from middleware, application, and database servers. DMZ controls are critical, as
these servers are exposed to the internet and, therefore, have a large threat footprint.
¡ Restrict the ability for DMZ servers to log directly into inside network servers, specically using
remote desktop protocol, server message block, SSH, or other remote access ports (tcp/3389,
tcp/445, tcp/139, tcp/22).
¡ Ensure local administrator passwords are unique to each DMZ server and do not use these
passwords for any other server in your organization.
¡ Ensure DMZ servers cannot connect directly to the internet. Instead, these servers should access
the internet through outbound proxy services. Outbound proxy rules should limit the sites,
URLs, IPs, and ports that a DMZ server can access to only allowlisted sites required for updates
or application functionality. Be cautious of allowlisting hosting organizations like Amazon Web
Services, as malicious actors may use them to download malware to a compromised server.
¡ Do not provide access to the internal network directly via protocols like telnet, SSH, or RDP.
Instead, leverage a VPN with MFA for accessing internal network resources.
¡ Consider this type of restriction conguration for partner WAN links or site-to-site VPN
connections. Do not permit access to systems/applications that are not required by the user.
• Data center networks: Servers in the data center should be segmented into appropriate zones.
Several different layers of segmentation may occur within data center networks, including
¡ database servers;
¡ application servers; and,
¡ middleware.
• Critical IoT assets: It is important to restrict access to assets that have a potentially high impact on
the business or patients if compromised. Management and patching of security vulnerabilities in
IoT devices is often limited. Examples include medical devices, security cameras, badge readers,
temperature sensors, and building management systems. These assets generally exist outside of
the data centers. Without proper segmentation, they may inltrate general access networks. To
achieve segmentation in physical buildings, leverage multiprotocol label switching to build out virtual
networks. Place these network access restrictions behind core rewalls.
• Vendor access: Vendor access should be limited based on need. It should be temporary, and only
access to required information should be granted. Some assets are managed exclusively or accessed
by third-party vendors. These vendors may need continual access to your organization’s network.
It is important to segment this vendor access from other networks and limit the vendor’s ability to
access other parts of your corporate network. Whether these networks exist inside or outside of the
data center, the principles are the same. In 2015, the retailer Target was the victim of a cyber-attack
56 “CIS Critical Security Control 12: Network Infrastructure Management,” Center for Information Security Controls
(Accessed June 2, 2022), https://www.cisecurity.org/controls/boundary-defense/.
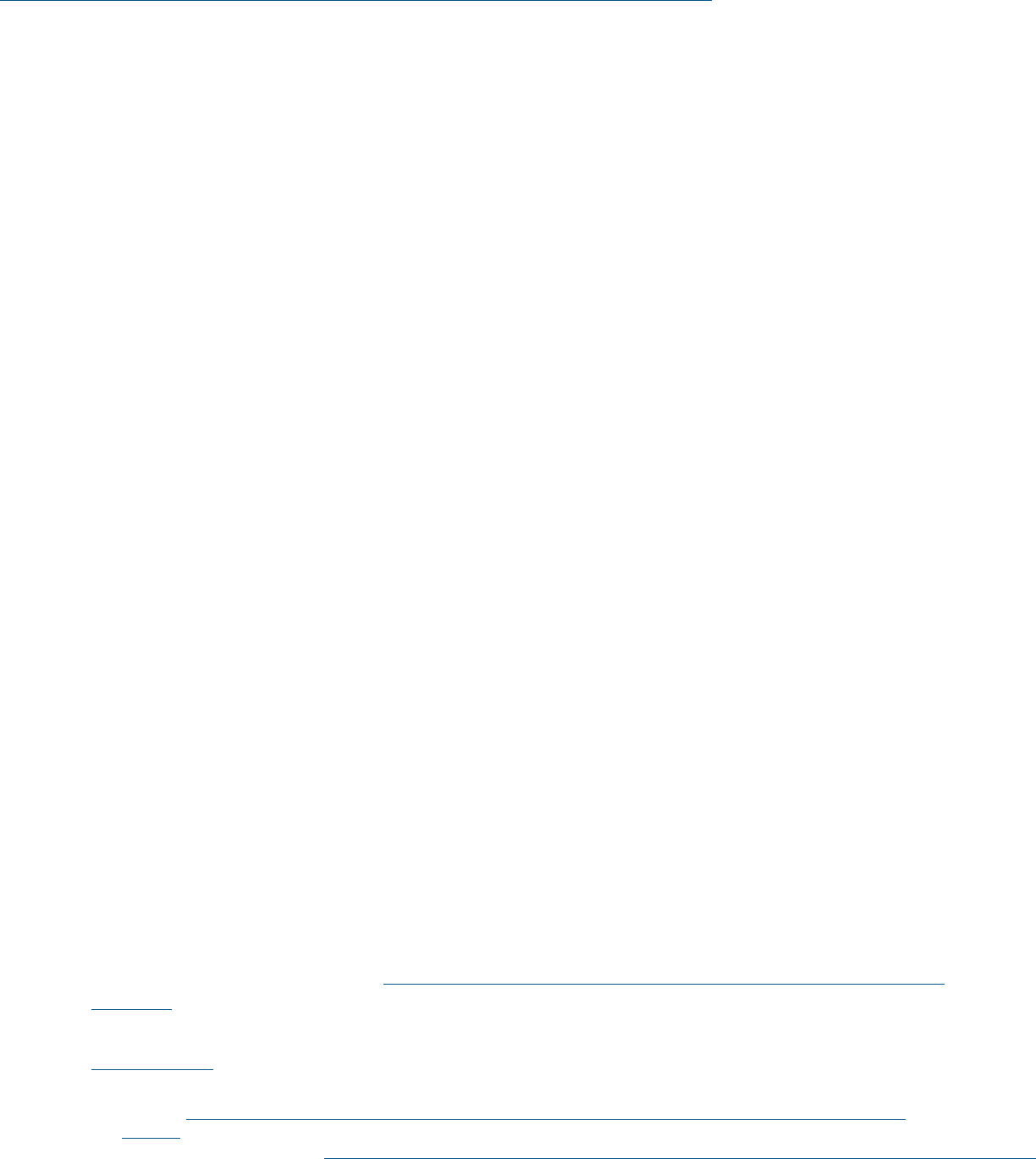
Cybersecurity Pracce #6: Network Management
66Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
leveraging these channels.
57
Common examples include building management systems, security
systems, physical access controls, and persistent tunnels required to enable cloud functionality.
• General access networks: Most of your workforce will operate on general access networks. These are
“edge” networks that provide connectivity back to the services offered in data centers, the internet,
or other assets. General access networks require a sense of openness when communicating with
services that are hosted by your organization. However, restrictions should be implemented that
prohibit the assets in one general access network from communicating with the assets in another
general access network. This critical control that can help stop the outbreak and spread of malware
and ransomware attacks.
• Payment Card Processing networks: Establishing a dedicated zone specically for systems processing
credit card data will limit the scope of PCI compliance obligations and minimize cardholder
data exposure.
• Guest networks: It is common for organizations to provide guest access to the internet, especially
in provider organizations visited by patients and their friends and families. However, it must be
restricted and controlled appropriately. These restrictions should exist on wireless networks (where
it is most common), as well as wired networks often located in public spaces or conference rooms.
Explicitly prohibit access to the internal network from networks. Guest users requiring access to
internal resources should leverage a publicly available website or VPN. To the extent possible, limit
the ability of your workforce to access guest networks. Guest networks may not have the same
controls as your internal network.
6.M.C: Intrusion Prevention Systems
NIST Framework Ref: DE.CM-1
An intrusion prevention system (IPS) is important for your network perimeter, data center, and partner
connections. An IPS is capable of reading network trafc to detect and potentially prevent known attacks.
IPS will typically leverage deep packet inspection to look at the context of protocols.
Increasingly, IPS is integrated with next generation rewalls and are not often found as a standalone
device. When deploying IPS systems for the rst time, it is recommended to enable them into a ‘monitor
only’ mode so they system can be properly tuned without causing disruptions. When the tuning is
complete, you can then enable them in “prevention mode” or “quarantine mode” to proactively stop
malicious attacks.
Savvy attackers will take steps to obfuscate or mask malicious trafc to avoid detection. To stay up to
date, IPS should leverage a Structure Threat Information eXpression (STIX)/Trusted Automated eXchange
of Indicator Information (TAXII) feed to obtain IOC from an Information Sharing and Analysis Center
(ISAC) or similar source. While an IPS may not identify every single attack, it can be useful for baselining
your network activity (as covered in Cybersecurity Practice #8: Security Operations Center and Incident
Response). An IPS may also provide information enabling your IR team to conduct forensic activities.
57 Michael Kassner, “Anatomy of the Target data breach: Missed opportunities and lessons learned,” ZDNet (February
2, 2015), https://www.zdnet.com/article/anatomy-of-the-target-data-breach-missed-opportunities-and-lessons-
learned/.

Cybersecurity Pracce #6: Network Management
67Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
6.M.D: Web Proxy Protection
NIST Framework Ref: PR.AC-3, PR.AC-5
Web proxy systems provide important protections against phishing and malware attacks. These systems
are implemented at the perimeter of the network or in the cloud to provide protections for your mobile
workforce. Because most phishing and malware attacks are web-based, web proxy systems provide user
friendly error pages explaining that they have been restricted from accessing a known malicious website.
Such pages also provide informative feedback for users. When congured properly, web proxy systems
leverage the following methods to limit client-side attacks:
• Reputation blocking: Many blackhole lists are available publicly or through Information Sharing and
Analysis Centers (ISACs) and Information Sharing and Analysis Organizations (ISAOs); proxies can
use these lists to prevent users from accessing malicious websites. The lists are usually integrated
into proxy systems through automated feeds.
• Organizational block lists: As part of an organization’s IR, malicious websites and other sites can be
identied based on actual attacks against your organization. Web proxy systems are critical shut-off
points to limit access to websites quickly.
• Category blocking: Most modern, commercial web proxy technologies will pre-categorize websites
on behalf of your organization. Considering the millions of websites that exist, this is a highly useful
service. Consider blocking categories that contain malicious, suspicious, or illegal websites.
In addition to blocking trafc to specic sites, web proxies can inspect TLS trafc. This is important since
over half of all malicious trafc is sent encrypted. Unencrypting HTTPS trafc allows:
• the data to be checked for malicious content;
• downloads to be sandboxed prior to delivery; and
• other functions to occur that reduce the likelihood of web-based attacks and compromise.
Sandboxing is one function of a web proxy. Through monitoring common protocols that allow
downloading of binaries and les, organizations can check a download prior to permitting it to run on
your organization’s devices. Downloaded binaries, executables, or even data les (e.g., docx, xlsx) run
in a virtual environment that looks for malicious activities when the le executes. Tools that facilitate
automated sandboxing look for suspicious outputs or actions, rather than attempting to base actions on a
particular signature of a specic conguration.
Web proxies and similar infrastructure can inspect les, and other content, passively or actively. Passive
systems monitor network trafc at the stream level, not residing in line with the communication ows.
Active systems insert themselves into the communication ows and conduct checks automatically,
denying access to downloaded les until they are cleared.
Cybersecurity Pracce #6: Network Management
68Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
6.M.E: Physical Security of Network Devices
NIST Framework Ref: PR.AC-2
Network devices are deployed throughout an organization’s facilities. Inside the general user space,
physical data closets that contain network devices must be secured. Additionally, it is useful to limit
network ports on switches. Consider the following controls:
• Data and network closets should always be locked. Consider the installation of badge readers instead
of traditional key locks to monitor access.
• Disable network ports not in use. Ensure procedures are in place to maintain ports in shutdown mode
(until an activation request is submitted and approved).
• Establish guest networks in conference rooms congured to access specic networks that do not have
access to individually identiable information or other sensitive data.
Sub-Practices for Large Organizations
This section includes methods to detect and potentially prevent cyber-attacks against an organization’s
network. These methods should be engineered into network management practices. Once network-level
detection and prevention methods are established, cybersecurity departments can follow Cybersecurity
Practice #8: Security Operations Center and Incident Response to monitor and respond to attacks on
the network.
6.L.A: Additional Network Segmentation
NIST Framework Ref: PR.AC-5, PR.AC-6, PR.PT-4
Further limiting access to sensitive resources can lessen the potential impact of a security incident.
Consider the following additional segmentation approaches:
• Required VPN access for data center: Consider implementing a VPN, or bastion hosts, that must be
enabled before access is granted to privileged servers in the data center. The VPN/bastion hosts
should be equipped with MFA. Only authorized IT administrators should be granted access. Logs
should be routed to the SOC for monitoring.
• Zero Trust: One emerging framework for organizational cybersecurity is “zero trust.” This framework
has a basic design principle of “never trust, always verify.” In practice, this means a more active role
is taken in managing and granting access to network resources—continually verifying identities,
devices, and services. In contrast to the traditional perimeter security mindset, this framework is
designed to address the more fragmented nature of network use emerging in the past few years (as
due to home and mobile workers, network connected medical devices, employee-introduced mobile
devices, and network use by contractors and vendors). Zero trust is a framework used to deliver
a more granular segmentation of users, assets, and resources on your network. For example, in a
zero trust environment, a user afliated with HR would not be able to make a network connection
to a radiology system. This can help reduce the spread of malicious software like ransomware on
a network.
Cybersecurity Pracce #6: Network Management
69Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
6.L.B: Network Analytics and Blocking
NIST Framework Ref: DE.CM-1, DE.CM-7
Advanced persistent threats (APT), botnets, backdoors, and other technically sophisticated attacks may
leverage concealed or camouaged network trafc to bypass typical network protections. This includes
command and control (C2) trafc to maintain access to compromised computers. C2 trafc consists of
beacons, typically outbound from the computer, that check back into a central server. Identifying such
trafc can help detect where an attacker has maintained persistence. Signs of C2 trafc include:
• Direct to compromised server via Internet Protocol (IP) or Internet Control Message Protocol (ICMP):
Trafc runs over the network using outbound ports or protocols that are generally open (e.g., HTTP,
HTTPS, or ICMP protocols).
• DNS queries: The attacker establishes control using a DNS query embedded in malware that
is downloaded to a computer. If the DNS record is maintained, the servers that maintain C2
communications can switch out and ex as they are discovered.
• Fast ux DNS queries: The hacker leverages DNS to maintain persistence, knowing that the DNS
registrations will likely be taken down at some point. When this occurs, malware downloaded to the
local client and C2 services runs an algorithm that checks the rst several bytes of well-known sites
(e.g., cnn.com, nbc.com) to create and register fake DNS names on your organization’s DNS resolvers.
To effectively address C2 trafc and other potential malicious activity, the best approach is to analyze
network trafc rather than focus on a particular vector or attack style. Network tools may support
“deep inspection,” which allows the full contents of a packet to be analyzed, categorized, and built into
massive databases of network-based metadata. Since trafc may not be easily detected, multiple
different methods may be used together including:
• Intrusion Prevention System: As noted in cybersecurity practice 6.M.C: Intrusion Prevention Systems,
an IPS combined with IOC can identify trafc to known command and control servers as well as
common methods highlighted above.
• Netow: Solutions exist that can leverage netow data (e.g., source, destination, protocol) can
perform analytics to look for anomalous activity (e.g., infusion pump communicating over DNS to an
internet server).
• Next generation rewall: These devices can prole trafc and help monitor and block
persistence mechanisms.
After metadata on the network trafc prole is gathered, analytics can be conducted to look for outliers,
anomalous trafc, and other highly sophisticated methods of discovery. Network monitoring tools are
not preventative in nature. Rather, they are intended to widely increase the SOC’s visibility, facilitating
detection, conrmation, or validation of suspicious actions. These tools are especially useful in replaying
events that occurred as part of an attack to support network forensic activities. To block C2 trafc and
other malicious network activity, consider using:
• DNS ltering: DNS providers will automatically block connections to known command and control
servers (as well as DNS based persistence mechanisms), instead of allowing computers to leverage
any authoritative DNS source.
• Egress ltering: Allowing the minimum necessary outbound protocols to restrict the ability of C2
trafc to blend into background.

Cybersecurity Pracce #6: Network Management
70Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
6.L.C: Network Access Control (NAC)
NIST Framework Ref: PR.AC-5, PR.AC-6, PR.AC-4
NAC systems are engineered to automatically prole new IT assets that connect to network resources.
Examples include wireless networks, wired networks, or VPN. NAC systems execute these controls in real
time when the asset connects to the network. Common NAC use cases include:
• Discovering personal devices (i.e., BYOD) leveraged on the network. They can be congured to permit
authorized BYOD devices to access the network or prohibit them entirely.
• Authenticating users associated with devices to conrm no authorized access of the network.
• Quarantining connected devices that do not meet your organization’s minimum standards. For example,
they help ensure that the controls discussed in Cybersecurity Practice #2: Endpoint Protection
Systems are in place on each asset.
• Implementing granular network segmentation. As devices are connected to the network, they can be
automatically added to the correct VLAN to limit communication.
• Isolating affected devices from the rest of the network. This can take place during an incident
(e.g., ransomware).
• Integrating with other systems (e.g., rewall, ITAM repository, SIEM). This provides greater visibility of
connected devices.
As discussed in Cybersecurity Practice #5: IT Asset Management, ITAM repositories should be populated
using your organization’s standard procurement processes. That said, not all processes run perfectly.
There are other ways that assets are integrated into an organization’s environment, often due to human
error or sidebar procurement channels that are not leveraged consistently.
Conguring your NAC solution to check against your ITAM enables assets to be proled spontaneously,
providing self-directed work streams to users. Use the following steps to achieve this type
of conguration:
• Set up application programming interfaces between the NAC solution and the ITAM solution that
enable read and write options.
• Query the ITAM database when an asset connects to the network. If the asset does not exist, present
the user with a splash page.
• Determine whether the asset is owned by your organization or a personally owned device.
• Register the selection, conduct the NAC security scan, and publish the results in the ITAM.
• Execute IT general controls that reconcile assets that are out of compliance with standard asset
management procedures. Such controls can include:
¡ ensure that appropriate monitoring controls are in place;
¡ register the asset with the right identiers (asset IDs); and
¡ update asset ownership based on actual human interaction.
These mechanisms are effective at providing visibility to the devices being used on the network,
increasing the ITAM system’s accuracy and consistency.
Cybersecurity Pracce #6: Network Management
71Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Key Mitigated Threats
1. Ransomware attacks
2. Loss or theft of equipment or data
3. Insider, accidental or malicious data loss
4. Attacks against network connected medical devices that may affect patient safety
Suggested Metrics
• The amount of time since last review of rewall and network segmentation congurations, reviewed on a
weeky basis. The goal is to have a regular process to review and validate existing rewall and network
settings, but also search for any undocumented rewalls or network segments.
• Number of assets on the network that have not been categorized, measured weekly. The goal is to
establish a process to register and understand all assets on the network. After the baseline is
complete, minimize the number of uncategorized assets.
• Number of organizationally owned assets discovered using NAC that were not previously categorized
through asset management procedures, measured monthly. The goal is to monitor this lagging
metric that measures effectiveness of the supply chain and IT operations processes. Increases in
the number of organizationally owned assets not previously categorized indicates that standard
processes are not being executed properly. Implement continuous improvement processes for
IT operations.
• Percentage of assets that comply with security policies, measured weekly. The goal is to establish
a baseline, then set stepwise goals to improve compliance over time. Ultimately, compliance
percentage should range from 95 to 99 percent.
• Number of malicious les captured and secured with advanced networking tools (sandboxing), measured
weekly. The goal is to capture all malicious les. An extended trend of no detected malicious les may
indicate that sandboxing solutions are not working.
• Number of malicious C2 connections discovered and removed, measured weekly. The goal is a weekly
report showing that all detected C2 connections are mitigated successfully.
• Number of approved servers/hosts in the DMZ compared to hosts in the DMZ, measured weekly. The
goal is zero servers/hosts in the DMZ that are not understood. IT operations practices should be
reviewed if servers are added that were not previously authorized.
72Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #7:
Vulnerability Management
Areas of Impact
PHI
Medium Sub-Practices
7.M.A Host/Server Based
Scanning
7.M.B Web Application
Scanning
7.M.C System Placement and
Data Classication
7.M.D Patch Management,
Conguration
Management
7.M.E Change Management
Large Sub-Practices
7.L.A Penetration Testing
7.L.B Vulnerability
Remediation Planning
7.L.C Attack Simulation
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Attacks against network
connected medical
devices that may affect
patient safety
405(d) Resources
• Prescription Poster:
Vulnerability Management
Organizations use vulnerability management for the proactive
discovery of vulnerabilities. These processes enable your
organization to classify, evaluate, prioritize, remediate, and
mitigate the technical vulnerability footprint from the perspective
of an attacker. The ability to mitigate vulnerabilities before a
hacker discovers them gives your organization an operational
advantage by providing time to address these vulnerabilities in a
prioritized fashion.
58
There are multiple types of vulnerability scanning. The most well-
known methods are scans against servers (or hosts) and against web
applications. These two scan types focus on different considerations.
Sub-Practices for Medium-
Sized Organizations
7.M.A: Host/Server-Based Scanning
NIST Framework Ref: DE.CM-8
Vulnerability scanners are leveraged to identify weaknesses in
operating systems or third-party applications that reside on a server.
There are two scan options: unauthenticated and authenticated.
When performing unauthenticated scans, the scanner software does
not have server privileges. The scan is performed through queries
of the server based on ports that are active and present for network
connectivity. Depending on the level of sophistication of the software scanner, each server is queried and
checked for vulnerabilities. Scan results provide the perspective of an attacker who lacks server access.
Vulnerabilities that rate high in this space should be mitigated rst, as they are the most likely points at
which a hacker could enter the server.
Authenticated scans are conducted by letting the vulnerability scanner log in to the server and query all
active software with all running versions. The resulting vulnerability lists are usually compared against
a database maintained by the scanner’s vendor. Vulnerabilities are enumerated based on the known
software version’s disclosed issues.
Authenticated scanning provides a much higher degree of accuracy in enumerating vulnerabilities. It
does not necessarily provide context that describes how the vulnerabilities might be exploited. Another
58 “Common Vulnerability Scoring System version 3.1: Specication Document,” FIRST (Accessed June 2, 2022), https://
www.rst.org/cvss/specication-document.

Cybersecurity Pracce #7: Vulnerability Management
73Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
advantage of the authenticated scan is that it will identify client-side vulnerabilities that exist on the
server that may otherwise be difcult to discover (e.g., vulnerable versions of Java).
Most scanning systems can categorize vulnerabilities against the MITRE Common Vulnerability Scoring
System (CVSS). The CVSS system helps organizations prioritize identied vulnerabilities, which enables
development of a prioritized response. Version 3 of the CVSS system considers three factors: base
score, temporal score, and environmental score. These factors, along with their sub-factors, are used
to calculate vulnerabilities on a low-to-high scale range from 1 to 10. For more information, refer to the
CVSS Specication Document.
59
7.M.B: Web Application Scanning
NIST Framework Ref: DE.CM-8
Specialized vulnerability scanners interrogate a running web application to check for vulnerabilities in
the application design. Most web applications run dynamic code, run atop a web server, interact with
middleware, and connect to databases. If the web application is not coded securely, this architecture may
enable unanticipated access to data or systems.
Common web application attack types include Structured Query Language (SQL) injection, cross-site
scripting, and security miscongurations. In these cases, attackers can:
• bypass web application security controls and pull data directly from the database
• steal an already authenticated cookie on a vulnerable website to get access
• exploit miscongurations that can permit properly formatted commands or scripts to execute
privileged content on the webserver itself
More information can be found on the Open Web Application Security Project’s (OWASP) Top
10 website.
60
In all cases, vulnerabilities to web applications with sensitive information represent a high risk to
your organization. It is important to understand these vulnerabilities to conduct appropriate and
prioritized remediation.
7.M.C: System Placement and Data Classication
NIST Framework Ref: ID.RA-5
Organizations should apply Cybersecurity Practice #4: Data Protection and Loss Prevention and
Cybersecurity Practice #5: IT Asset Management to understand IT assets and asset classications.
These cybersecurity practices answer the question, “How bad would it be if this asset were breached?”
It is important to understand the exposure of each system in your environment. Organizations should
apply Cybersecurity Practice #6: Network Management to determine the likelihood that a system can
be compromised.
59 “Common Vulnerability Scoring System version 3.1: Specication Document,” FIRST (Accessed June 2, 2022), https://
www.rst.org/cvss/specication-document.
60 “OWASP Top 10 - 2017: Ten Most Critical Web Application Security Risks,” OWASP (2017), https://raw.
githubusercontent.com/OWASP/Top10/master/2017/OWASP%20Top%2010-2017%20(en).pdf.
Cybersecurity Pracce #7: Vulnerability Management
74Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
The level of risk related to vulnerabilities in your systems is directly related to the exposure of these
systems and the types of data they contain.
When establishing your vulnerability management program, consider the above practices for the
identication of risks and their impacts. The following scenarios are cases where risks should be ranked
higher, and remediation should be prioritized for vulnerabilities discovered:
• Internet-exposed, highly sensitive systems
• Systems necessary for life safety and patient safety
• Internet-exposed systems used for remote access
• Vendor-managed systems used for remote access
7.M.D: Patch Management, Conguration Management
NIST Framework Ref: PR.IP-1, PR.IP-3, PR.IP-12
All organizations should have a routine procedure to patch security aws in their servers, applications
(including web applications), and third-party software. Although the patching process may vary, large
organizations should use centralized systems to interrogate servers and determine which software
updates should be implemented.
At least monthly, organizations should implement patches that are produced by the vendor community. IT
operations should collect these patches, conduct appropriate regression tests to ensure that patches do
not negatively impact the business, and schedule patch implementation during routine change windows.
This process should be executed and measured using standard IT operations activities.
Not all vulnerabilities are created equal. Some are easier to exploit than others. The National
Vulnerability Database (NVD) has produced the CVSS, a standard measurement across all industries that
normalizes and ranks the severity of a vulnerability.
61
The more a vulnerability is exposed, the higher priority an organization will generally assign to mitigate
it. Exposure may be a more critical variable than the potential impact to an asset, considering that
hackers attempt to gain a foothold on organizational assets before conducting additional internal attacks.
Another factor to consider is the level of active exploitability. A less-critical vulnerability may have an
active threat against it. In such a case, an organization might want to consider proactively executing IR
processes, organizing the response team, and quickly patching systems. The WannaCry exploit of 2017
is a classic example of an organization identifying an active threat and quickly implementing previously
neglected patches.
62
If your information systems are running end-of-life operating systems or software, associated
vulnerabilities should be identied, and steps taken to bring these systems back to a supported state. This
may include decommissioning systems that run on unsupported operating systems, which may require
additional investments. Once systems are unsupported, it is usually impossible to apply security patches,
potentially increasing your organization’s risk.
Table 9 below provides general guidelines for planning remediation efforts based on criticalities.
61 “National Vulnerability Database: CVSS,” NIST (Accessed September 24, 2018), https://nvd.nist.gov/vuln-metrics/cvss.
62 Brandon Vigliarolo, “Report: The IT Response to WannaCry,” TechRepublic (July 25, 2017), https://www.techrepublic.
com/article/report-the-it-response-to-wannacry/.
Cybersecurity Pracce #7: Vulnerability Management
75Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 9. Recommended Timeframes for Mitigating IT Vulnerabilities
Vulnerability Cricality Days to Migate in DMZ Days to Migate in Data Center
Critical < 14 days < 30 days
High < 30 days < 90 days
Medium < 90 days < 180 days
Low < 180 days At your discretion
The vulnerability scanning process is a quality check on the effectiveness of an organization’s patch
management practice, otherwise referred to as a lagging metric. Organizations with a robust patch
management practice are better positioned to mitigate residual vulnerabilities.
In addition to conducting routine patch management activities, organizations should ensure that proper
security conguration management activities are in place. Common vulnerabilities can be introduced
in systems with insecure congurations. Examples of insecure congurations include permitting a le
transfer protocol (FTP) server to allow anonymous login, making that login credential accessible to the
internet, or failing to change default account passwords on applications. According to the 2020 Verizon
Data Breach Report, in 2020, more than 40% of breaches analyzed were due to conguration errors.
This failure has been trending upwards since 2015, where just less than 10% of breaches were due to
conguration errors.
63
Organizations that follow Cybersecurity Practice #2: Endpoint Protection
Systems (and expand these practices to their servers) will be positioned to minimize these issues.
7.M.E: Change Management
NIST Framework Ref: PR.IP-1, PR.IP-3, PR.IP-12
When changes are made to information systems, they should be conducted in a controlled manner
to minimize disruption and outages made by human error. This process also allows for changes to
be reviewed by a Change Advisory Board (CAB) to ensure the change would unwittingly expose the
information system to an unacceptable vulnerability.
There are multiple types of changes that could occur in an organization. If following standard Information
Technology Infrastructure Library (ITIL) practices, you could break these changes into normal changes,
standard changes and emergency changes.
• Normal system change: This type of change is what most people think of when they go through
the change process. This is a change that is made to an information system to enhance a feature,
maintain the system, or otherwise update its services or congurations. These types of changes are
planned out and prioritized.
• Standard system change: A subset of normal changes, standard changes are those that are recurring,
routine and very specic. These changes have a standard operating procedure and have been
conducted on a regular cadence, proven to cause minimal to no disruption as risks are known upfront.
Standard changes offer exibility to an organization once they have demonstrated to be stable.
They can be pre-determined on a schedule, approved ahead of time by CAB so they do not need an
approval every time, and otherwise permit standard exibility.
63 2020 Data Breach Investigations Report (DBIR), Verizon (2020), https://www.verizon.com/business/resources/
reports/dbir/2020/.

Cybersecurity Pracce #7: Vulnerability Management
76Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Emergency system change: Emergency changes are changes that must happen immediately due to
the unavailability of an information system or service, or perhaps due to an imminent outage. These
types of changes need to occur immediately and without the standard approval process, but still must
be controlled carefully. Emergency changes should be few and far between, measured, and require
an after-action review for each emergency change that occurred.
All changes, regardless of their type, should be reviewed by a CAB. In some cases (i.e., standard changes),
the CAB can approve the change to reoccur on a set schedule after it has been determined to be a stable
and repeatable process. Other changes, such as emergency changes, might not go to the CAB prior to
implementation, but must be discussed after the change has been made.
A CAB should have representation across your IT division. It is not just the responsibility of the person
implementing the change to review it. Each department within your IT division should weigh in and
review the impact of the change to ensure the stability of the digital environment. Cybersecurity teams
should provide specialized insight to the change and make sure it will not introduce a vulnerability that is
unacceptable to your organization.
A change ticket should capture, at a minimum, the following elds:
• Implementation Plan: The change must describe, with sufcient level of detail, the steps that will be
taken to implement the change requested. The detail must be robust enough to allow for members of
the CAB to make an informed decision. Consider placing a vulnerability scan as part of your testing
plan to ensure no new vulnerabilities were introduced. These vulnerability scans should be done
within the test environment and made prior to the change being implemented into production.
• Testing Plan: The change must incorporate a plan on how to test that the change was successful.
Every change should have a test plan to validate its effectiveness.
• Back-out Plan: Not all changes are successful, so you must plan for how you will reverse the change
and bring the information system back up to its current state. No change should take place without
an approved and tested Back-out Plan.
• Communication Plan: Changes should include the mechanisms by which you will communicate how
the change was completed, new features being released, and new adjustments that are necessary by
your organization to adjust to the change that was introduced.
Sub-Practices for Large Organizations
7.L.A: Penetration Testing
NIST Framework Ref: ID.RA-1, PR.IP-12, DE.CM-8, RS.AN-5
Penetration testing is an important tool that layers additional protections when added to vulnerability
scanning. Penetration testing is sometimes called “red-teaming”. The goal is to actively exploit your own
environment before malicious actors do.
Penetration tests involve more than simply conducting vulnerability scans and attempting to exploit the
ndings. A proper penetration test should mimic the same attack methodologies that are deployed by
the adversaries. CIS Control #18 tells us penetration testing involves mimicking the actions of computer

Cybersecurity Pracce #7: Vulnerability Management
77Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
attackers to identify vulnerabilities in a target organization and exploiting them to determine what kind of
access an attacker can gain. Penetration tests typically provide a deeper analysis of security aws than a
vulnerability assessment.
64
Penetration tests should blend client-based, internet-based, web application–based, and wireless-
based attacks. When selecting a testing method, consider the types of attacks that might occur
most frequently against your organization. With these scenarios, you can test the resiliency of your
cybersecurity program.
Penetration tests can be run internally by qualied individuals, or they can be run by external partners.
No matter who will conduct the test, proper authority to perform the test must be documented. This
must clearly dene the scope of the assets that may be tested, the methods that may be deployed, and
the timing for conducting the tests. Assets and methods not permitted should be clearly articulated. This
documentation is especially important if internal staff will conduct the test, and documentation may be
necessary to comply with legal and HR obligations.
Multiple variations of penetration tests that can be conducted. Review each of the factors in Table 10
below and select what works best for your organization.
Table 10. Factors for Consideration in Penetration Test Planning
Factor Opons Descripon
Type 1. White box: Tester is permitted to know all
aspects of the target
2. Grey box: Tester is permitted to know some
aspects of the target
3. Black box: Tester is not permitted to know
any details of the target
Depending on the type of test you
want to conduct, it might be useful for
the tester to know some details of the
target or organization. Such knowledge
might reduce the effort of common
reconnaissance activities, such as
nding phishing target email addresses
or discovering all vulnerabilities on
externally facing servers.
Resources
1. External expert: A subject matter expert
(SME) who specializes in the specic
methodologies you wish to deploy
2. Internal expert: A SME on an internal team
who has context to the environment
Both types of resource can be useful.
The benet of using internal staff is that
they understand the technical nuances
of your environment. In some cases,
targeted tests requiring specialized
skillsets might be desired. External
experts are useful in these cases, or
when internal resources are committed
to other activities.
64 “CIS Critical Security Control 18: Penetration Testing,” Center for Internet Security (Accessed September 24, 2018),
https://www.cisecurity.org/controls/penetration-testing.
Cybersecurity Pracce #7: Vulnerability Management
78Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Factor Opons Descripon
Methods 1. Social engineering: Attacks geared towards
“tricking the human”
2. Web application: Attacks centered on
attacking web application infrastructure
3. Host based: Attacks focused on attacking
host infrastructure, inclusive of servers,
or endpoints
4. Client based: Attacks centered on attacking
the client, such as laptops or desktops (usually
bypassing perimeter protections)
5. Network based: Attacks against the network
infrastructure itself, such as physical
connections or wireless attacks
6. Privileged escalation: Once a foothold has
been made, conducting secondary attacks
to further escalate privileges for more
lateral movement
Many methods exist; those listed here
are the most common. These methods
can be combined, based on the type of
attack you are looking to carry out.
For example, if you want to see whether
it is possible for an external attacker to
gain access to your EMR, you might use
social engineering, client-based, and
privileged- escalation attacks. The goal
of each of these attacks is to discover
a user with sensitive EMR access,
compromise the user’s credentials, and
get remote access to the environment
to be able to log in to the EMR with
those credentials.
Targets
1. Data: Discover and exltrate sensitive data to
test data security controls
2. IT assets: Compromise IT assets, such
as servers or endpoints, to test system
security controls
3. People: Compromise individuals to test
educational controls
4. Medical technologies: Determine how
vulnerable your organization is to attacks
against medical devices. For additional clarity
on actions to be taken when vulnerabilities
are identied in medical devices, please refer
to Cybersecurity Practice #9: Network
Connected Medical Devices
5. Infrastructure: Determine how vulnerable
your organization is to digital extortion
attacks, such as ransomware outbreaks
Each test conducted should have
different targets and goals in mind. In
some cases, you might want to test
how susceptible your user population
is to phishing attacks; in that case you
will set “People” as the target. In other
cases, you might want to understand
how vulnerable your organization
is to a ransomware attacks; in that
case, you might select “IT Assets” and
“Infrastructure” as your targets
7.L.B: Vulnerability Remediation Planning
NIST Framework Ref: PR.IP-12
It is important to classify and prioritize vulnerabilities that remain after completion of standard patch
management practices. Typically, these remaining vulnerabilities are issues that cannot be mitigated

Cybersecurity Pracce #7: Vulnerability Management
79Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
with a patch. They may require system conguration changes, code updates, or perhaps even a full-
blown version upgrade. The process of resolving these vulnerabilities tends to be more time-consuming
and complex.
Like risk management activities, remediation efforts should be prioritized to resolve identied
vulnerabilities. The most common practice is to rst patch identied vulnerabilities and then rescan the
system to validate that those vulnerabilities are closed. Most vulnerability scanning systems can track the
opening, closure, and reopening of vulnerabilities over time. It is highly encouraged to track these metrics.
Mitigation of some vulnerabilities requires far more effort than a simple patch. In these cases, it is best to
develop structured remediation plans, including the following elements:
• Plan owner: The single individual accountable for ensuring that the vulnerabilities are addressed. It is
important to assign remediation plans to a single owner, otherwise they are likely to stall due to lack
of leadership.
• Plan: A full description of the remediation plan to be completed. The remediation plan owner and
the cybersecurity ofce should develop this plan. Once the plan is approved, execution tasks can
be started.
• Stakeholders: The individuals responsible for completing tasks in the remediation plan or organizing
others who will complete tasks. Stakeholders may include those who need to be informed of
remediation activities and others who complete the work.
• Dates: Major milestone dates and remediation plan due dates must be captured on the remediation
plan. The remediation plan owner must commit to these dates.
• Status: Periodically, the plan should be updated to remain current. Updating generally occurs
between once per week and once per month. The remediation plan owner may be accountable for
providing status updates.
After a remediation plan is completed, your organization’s cybersecurity ofce should implement a
monitoring process. This monitoring process may include all remediation plans in progress and current
activities. The security ofce may provide support to activities that are behind schedule. Consider
implementing a monitoring process once per week to maintain momentum.
7.L.C: Attack Simulation
NIST Framework Ref: DE.DP
The last time you want to nd out about a vulnerability is during a cyber-attack. Attack simulations,
also known as threat emulation exercises, can help you expose your known and unknown vulnerabilities
and stress-tests your organization’s cybersecurity. The purpose of a threat emulation exercise is to
closely mimic the tactics, techniques, and procedures (TTPs) of real-world adversaries and determine
how they might be leveraged against your organization. There are a few important considerations that
organizations should consider when building a threat emulation exercise.
First and foremost, an organization needs to understand their own threat prole. Each organization has
a unique threat prole that is comprised of their internal mix of people, and processes, technologies. This
task requires an organization to develop a comprehensive understanding of their systems, applications,
networks, online presence, workforce, and the threat actors that focus on their industry. There are open-
sourced resources available to assist organizations in collecting this information. This task can be aligned
Cybersecurity Pracce #7: Vulnerability Management
80Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
to the reconnaissance and Open-Source Intelligence (OSINT) activities that normally happen as part of a
red team or penetration engagement.
Second, an organization will need to determine which framework and methodology to be used to conduct
the exercise. This will be the basis for how the specic parameters of the exercise will be carried out.
Additionally, the metrics of the exercise should also be based on the framework and methodology.
Lastly, an organization needs to determine the goals of the exercise. Once the goals are set your
organization can begin to build a threat prole. This includes identifying the specic TTPs of the
“attacker”, identify targets, develop real world scenarios, and determine the “attack” infrastructure
needed to achieve the goals they set for the threat emulation exercise.
When it comes to building a threat emulation exercise there are three phases that all the activities fall
under: Get in, Stay in and Act. The goals of these phases include activities such as:
• Acquiring elevated access to a domain controller or other critical servers.
• Accessing a client data repository, intellectual property, and/or application data.
• Creating a new cloud instance in the client’s on-premises or cloud infrastructure.
• Gaining access to and leaving a physical note in a datacenter or other restricted area.
• Posting a comment into production source code.
• Obtaining physical access to data or devices and accessing the ability to remove the data/device.
• Keeping a low prole (i.e., not generating alerts that will raise suspicions or having the attack
infrastructure get burned).
For additional guidance, there are several resources that offer options around attack simulation training.
The Identify, Mitigate, and Recover (IMR) incident response curriculum, developed by the Cybersecurity
and Infrastructure Security Agency (CISA), provides a range of training offerings for beginner,
intermediate, and advanced cyber professionals. It encompasses basic cybersecurity awareness and
best practices for organizations, live red/blue team network defense demonstrations emulating real-
time IR scenarios, and hands-on cyber range training courses for IR practitioners. Course types include
awareness webinars, Cyber Range Training, Cyber Range Challenges, and Observe the Attack.
65
• Cyber Range Training courses are hands-on labs designed to teach the basics of network investigation
and defense. They are accessible to new cybersecurity workers who may lack hands-on skill practice,
but some theoretical understanding of cybersecurity and IR enhances the value of the instruction.
• Cyber Range Challenges are hands-on IR scenarios designed for experienced practitioners. Students
are asked to complete class proles to summarize their skill and experience, and teams are balanced so
that newer incident responders can learn from and work with more experienced professionals. These
are critical thinking and problem-solving challenges as much as they are a test of investigation and
network defense skills.
• The Observe the Attack series red/blue team demonstration events are ideal for those who
supervise, manage, support, or facilitate incident or crisis response.
The Department of Homeland Security (DHS), the Department of Health and Human Services (HHS), and
the National Health Information Sharing and Analysis Center (NH-ISAC) developed a Cyber Tabletop
65 “Incident Response Training,” CISA (Accessed May 26, 2022), https://www.cisa.gov/incident-response-training#.
Cybersecurity Pracce #7: Vulnerability Management
81Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Exercise for the Healthcare Industry intended to assist healthcare industry organizations in planning and
organizing a cyber tabletop exercise.
66
CyberStorm, CISA’s biennial exercise series, provides the framework for the most extensive government-
sponsored cybersecurity exercise of its kind. The exercise series brings together the public and private
sectors to simulate discovery of and response to a signicant cyber incident impacting the Nation’s critical
infrastructure. CyberStorm exercises are part of CISA’s ongoing efforts to assess and strengthen cyber
preparedness and examine incident response processes.
67
An additional resource is the MITRE ATT&CK® framework. This is an open and publicly available
resource for understanding, planning, and designing attack simulations throughout the attack lifecycle.
Per their website: “MITRE ATT&CK® is a globally-accessible knowledge base of adversary tactics and
techniques based on real-world observations. The ATT&CK knowledge base is used as a foundation for
the development of specic threat models and methodologies in the private sector, in government, and in
the cybersecurity product and service community.”
68
Key Mitigated Threats
1. Ransomware attacks
2. Insider, accidental or malicious data loss
3. Attacks against network connected medical devices that may affect patient safety
Suggested Metrics
• Stacked aggregate of vulnerabilities in DMZ measured by month, with vulnerabilities categorized using
CVSS categories (Critical, High, Medium, Low, None) and plotted as a simple stacked bar. The goal is to
mitigate the most severe vulnerabilities rst, through patching and conguration management. Of
the remaining vulnerabilities, the most critical should be mitigated within 30 days. The total number
of vulnerabilities should be reduced over time.
• Stacked aggregate of vulnerabilities in data center measured by month, with vulnerabilities categorized
using CVSS scores and plotted as a simple stacked bar. The goal is to mitigate the most severe
vulnerabilities rst, through patching and conguration management. The total number of
vulnerabilities should be reduced over time.
• Number of unmitigated new vulnerabilities introduced into the environment, measured on a weekly
basis. The goal is to keep the number of new vulnerabilities as low as possible, dened by your
organization’s level of risk tolerance.
66 “DHS Cyber Tabletop Exercise (TTX) for the Healthcare Industry [Exercise Materials],” Homeland Security Digital
Library (2013), https://www.hsdl.org/?abstract&did=789781.
67 “Cyber Storm: Securing Cyber Space,” CISA (Accessed May 26, 2022), https://www.cisa.gov/cyber-storm-securing-
cyber-space.
68 MITRE ATT&CK® (Accessed May 26, 2022), https://attack.mitre.org/.
82Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Cybersecurity Pracce #8:
Security Operaons Center
and Incident Response
Areas of Impact
PHI
Medium Sub-Practices
8.M.A Security Operations
Center
8.M.B Incident Response
8.M.C Information Sharing and
ISACs/ISAOs
Large Sub-Practices
8.L.A Advanced Security
Operations Center
8.L.B Advanced Information
Sharing
8.L.C Incident Response
Orchestration
8.L.D Baseline Network Trafc
8.L.E User Behavior Analytics
8.L.F Deception Technologies
Key Threats Addressed
• Social engineering
• Ransomware attacks
• Loss or theft of equipment
or data
• Insider, accidental or
malicious data loss
• Attacks against network
connected medical devices
that can affect patient safety
405(d) Resources
• Prescription Poster:
Incident Response
Most cybersecurity programs begin by implementing controls
designed to prevent cyber-attacks against an organization’s IT
infrastructure and data. This is a good place to start and there is a
lot of value in basic cyber hygiene, implementing the cybersecurity
practices that are discussed in this volume. However, in the modern
age of cyber threats, not all attacks can be prevented with these basic
controls. It is equally important to invest in and develop capabilities
to detect successful attacks and respond quickly to mitigate the
effects of these attacks.
A good example is the threat of phishing attacks. Even if
organizations followed every practice discussed in Cybersecurity
Practice #1: Email Protection Systems, they would still be
susceptible to phishing attacks. It is therefore important to detect,
in near-real time, phishing attacks that successfully inltrate your
environment and to neutralize their effects before widespread theft
of credentials or malware installation occurs. This is a classic example
of what it means to shore up your detection capabilities (detecting
the phishing attack that gets past your basic controls) and response
capabilities (neutralizing the effects before serious damage to your
organization occurs).
Maintaining detection and response capabilities requires establishing
an IR program and an SOC to manage the IR, along with security
engineering that enhances an organization’s ability to detect and
respond to cyber-attacks.
Sub-Practices for
Medium-Sized Organizations
8.M.A: Security Operations Center (SOC)
NIST Framework Ref: RS.RP
A SOC is an organizational structure that leverages cybersecurity frameworks, people, tools, and
processes to provide dedicated cybersecurity operations. SOCs are the areas within an organization
that dedicate 100 percent of their time to cybersecurity prevention, detection, or response capabilities,
providing the execution arm of cybersecurity IR. A SOC is generally segmented into three main functions,
depending on your organization’s level of maturity. These functions are as follows:
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
83Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Operations: The process of managing and maintaining the cybersecurity tools within the SOC. This is
sometimes referred to as ‘keeping the lights on’. ‘Keeping the lights on’ generally means monitoring
critical cybersecurity systems to ensure that they operate at agreed-upon performance levels.
• Threat intelligence: A specic function that focuses entirely on how to discover cybersecurity threats
that may be relevant to your organization, along with the means and methods these threats may use
to inltrate your organization. This function focuses on the threat actors themselves, the tools they
leverage, and the digital signatures they leave in the process of conducting their activities. Upon
establishing these digital footprints, sometimes called IOCs, engineering teams can integrate IOC
patterns into cybersecurity systems. IR plays can be set to execute when the IOCs are activated.
• Incident response: The process of conducting a structured and consistent response to any IR plays
that have been created. The goal of this function is to:
¡ validate an IR process that has been triggered;
¡ contain any successful cybersecurity attacks to your organization;
¡ eliminate the threat from the environment;
¡ recover systems or data that might have been affected by the attack; and
¡ ensure that any attack vectors that were exploited are well understood and fed back to the security
engineering teams for future prevention or enhanced detection capabilities, further minimizing the
impacts of those vectors.
Supporting the SOC is the cybersecurity engineering function. This team builds new cybersecurity
capabilities into the existing toolsets in an environment. Examples include building new alerts within
a SIEM system, establishing new log sources for log management systems, establishing new analytics
patterns for detection, or simply implementing new cybersecurity systems to add capabilities into the
environment. Additionally, the cybersecurity engineering team may take the lessons learned from the
SOC to improve your organization’s preventative and detective controls.
It is critical to create a continuous feedback loop between your SOC and cybersecurity engineering teams,
so your organization continues to learn and grow based on the actual success of threats and threat actors.
As SOCs are developed, a core concept is to ensure that IR teams and handlers apply consistent methods
to execute response practices. SOCs and IR teams should establish playbooks, also known as runbooks,
that describe existing detection mechanisms and the procedures to be followed if the mechanisms are
triggered. For each detection, the triggered process may be referred to as a play, like plays that football
teams maintain in their playbooks.
Examples of plays that might be found in an IR playbook are provided below in Table 11. The table
provides high-level play details, including what the play seeks to accomplish and the types of source data
that must be collected to successfully detect it. The list below will not discuss specic technical log event
data required. Information on how to congure this information can be found in multiple publications.
69
69 David Swift, Successful SIEM and Log Management Strategies for Audit and Compliance, The SANS Institute (November 9,
2010), https://www.sans.org/reading-room/whitepapers/auditing/successful-siem-log- management-strategies-audit-
compliance-33528.
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
84Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 11. Example Incident Response Plays for IR Playbooks
Play Category Play Descripon Source Data
Reconnaissance Vulnerability
scanning
sweep of DMZ.
Large numbers of vulnerabilities
are scanned across the DMZ
spectrum. Could involve scanning
a single server over multiple ports
or scanning multiple servers on a
single port.
• Server list in DMZ
• Intrusion detection
system (IDS) or intrusion
prevention system (IPS)
logs congured to detect
vulnerability scanning
• Firewall logs
• Netow data
Reconnaissance Vulnerability
scan from
known
malicious IPs.
Vulnerability scans of the DMZ or
other servers/endpoints exposed to
the internet over channels that are
shared and known to be malicious
(e.g., IOC).
• IOC list from threat-
sharing sources (e.g., ISACs)
• IDS/IPS logs
• Firewall logs
• Netow data
Reconnaissance Successful
access from
known
malicious IPs.
Successful authentications from
known malicious IP addresses.
Authentications through standard
remote access channels (e.g., VPNs,
virtual terminals, jump boxes, or
other mechanisms).
• Authentication logs
• Firewall logs
• IOC list from threat-
sharing sources (e.g., ISACs)
Reconnaissance Internal
attacks from
third-party
VPNs.
Detection of attacks coming
through partnering third-party VPN
connections (e.g., organizations that
provide building automation).
• Firewall logs (from
segmented networks)
• IDS/IPS logs
• Authentication log
• EDR logs
Exploitation Phishing
attacks
successfully
delivered to
users.
Detection of phishing attacks by IT
systems, or users reporting phishing
attacks. Contain the issue by
blocking URLs provided, proactively
resetting passwords for users that
clicked, and conducting AV scans
against endpoints where malicious
attachments were opened.
• Email protection systems
• Firewall logs
• Web proxy logs
• Endpoint AV
management logs
• EDR logs

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
85Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Play Category Play Descripon Source Data
Exploitation Successful
ransomware
attack
Detection of ransomware attacks
that occur inside your organization.
These may be small outbreaks or
larger issues. Consider:
• Setting up detection alerts for
indicators of known ransomware
(AV, threat feeds, etc.)
• Setting up detection alerts
for symptoms of ransomware
attacks (such as large IOPs
on le systems, encryption of
large amounts of les, user
experience issues)
• Determining severity; lower
severity issues can be dealt with
operationally; high severity
issues should instantiate the
Cybersecurity Incident Response
Team (CIRT)
• Containing and
responding accordingly
• Recovering through backups (do
not simply clean a system with
an AV scanner, but rather rebuild
and reimage)
• File system logs
• Endpoint AV
management logs
• Firewall logs
• Web proxy logs
• Threat feeds
• Email security logs
• EDR logs
Persistence Creation of
local user
accounts on
static systems
Detection of a local user account
being created on an asset, such as
a Windows *nix server, where local
user account creations normally
do not occur. This may indicate
malicious activity.
• Logs from local servers
• EDR logs
Persistence After exploit
persistence
hold
Detection of malicious users
attempting to maintain permanent
access. Look for launch or
changing of scheduled tasks,
script downloads, and new
process creation.
• Critical server lists
• Known process baselines
• Logs from server task or
scheduled job management
• URL ltering logs by server
• EDR logs
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
86Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Play Category Play Descripon Source Data
Privilege
Escalation
Privileged
account brute
force success
Large number of invalid login
attempts followed by a successful
login to a known privileged account.
• Privileged account list
• Authentication logs (e.g.,
active directory, servers)
Privilege
Escalation
Default
account
password
guessing
Large number of invalid login
attempts followed by a successful
login to a known default
user account.
• Default account list
• Authentication logs (e.g.,
active directory, servers)
Privilege
Escalation
Interactive
login to service
accounts
Detection of a service account being
used as an interactive login (a user
logging in to a terminal session).
Service accounts should only be
used for applications or services.
• Service account list
• Authentication logs (active
directory, servers)
• EDR logs
Data
Exltration
Data transfer Detection of data transfers
occurring outside of your
organization from servers that
normally do not conduct such
activities. Must normalize/baseline
server network behavior and detect
anomalous activities off baseline.
• Netow data, or rewall
trafc prole data
• List of permitted remote
storage sites (e.g., box)
Data
Exltration
Lost/stolen
device
User reports that a device was lost
or stolen from their possession.
Conduct standard actions to
immediately reduce the impact,
including, at minimum:
• Issuing a device wipe and
remote lock
• Checking for last encryption
status in control systems
• Executing CIRT if device
is unencrypted
• Users
• Mobile device
management systems
• Endpoint conguration
systems
In each of the cases outlined in Table 11, the source data provided will include events or log information
that is critical to detect the play being constructed. Specialized security systems can ingest these logs and
apply pattern matching, rule matching, and analytics capabilities to specic events in the logs to call out
potential incidents of interest. These specialized systems are referred to as SIEM systems.
Besides cybersecurity specic responses, consideration should be given to potential incidents that have
a physical component as well. For example, ransomware could impact the controller for a prescription
drug dispenser, digital lock, etc. In these cases, IR needs to consider how critical functions will need to be
maintained and restored while the investigation and containment activities are being performed.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
87Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
8.M.B: Incident Response
NIST Framework Ref: PR.IP-9, RS.AN-1, RS.MI-1, RS.MI-2, RC
A basic and important function of a cybersecurity organization is the IR process. The IR process provides
your organization with standardized procedures to respond to cyber-attacks. The attack may be as simple
as an attempted phishing attack against users, or a highly sophisticated extortion attack that shuts down
digital operations. In both cases, from minimal to signicant impact, the organized manner of an IR is
critical to managing these threats.
Large-Scale Response
In parallel with establishing a response process inside of a SOC, it’s also advisable to create a large-scale
cybersecurity incident response plan in coordination with your emergency management and business
continuity teams. This large-scale response is designed to allow for the continuity of operations of
the business during a cyber-attack. Other useful tools in response planning includes leveraging the
ONC’s SAFER guides, and specically their downtime procedures recommendations.
70
Another useful
tool is CISA’s Table-Top Exercise (TTX) scenarios, which are helpful when exercising and testing your
large-scale plans.
71
This section does not outline all the elements of covering a large-scale response, but rather takes
elements from NIST’s Computer Security Incident Handling Guide and outlines some key roles and
responsibilities that can be tied into an organization’s larger Incident Command System.
72
In addition to these roles and responsibilities, it is advisable for organizations to have established disaster
recovery plans (DRPs) as well as downtime procedures, in the event of a large-scale disruption. Generally,
a structured IR process contains the following segments:
• Preparation: Before you respond to a cybersecurity incident, it is important to have policies,
processes, and procedures in place, including the following components:
• IR policy: A policy that denes the categorization and severity of incidents, the stakeholders involved
in IR, the roles and responsibilities of each person, the entry criteria when a security incident occurs,
and the person who oversees IR plays. The stakeholders that may play a role in IR could range from
the standard blocking and tackling personnel in IT operations to non-IT related professionals in such
diverse areas like privacy, legal, marketing, and public affairs for high-impact incidents. A template IR
policy is provided in Appendix G, Resources and Templates.
• Cybersecurity incident response team (CIRT): A pre-formed and “on the ready” group that knows how
to navigate issues when critical- or high-severity security incidents arise. This team develops and
manages your organization’s response. CIRTs are formed in the HPH sector when potential data
breaches occur, and your organization must manage the potential breach. It is important to identify
the incident commander, the most senior ofcial who will oversee managing cybersecurity incidents.
The incident commander is usually the Chief Information Security Ofcer (CISO) or equivalent. Note
70 “SAFER Guide: Contingency Planning,” ONC HealthIT (July 2016), https://www.healthit.gov/sites/default/les/safer/
guides/safer_contingency_planning.pdf.
71 “CISA Tabletop Exercises Packages,” CISA (Accessed May 31, 2022), https://www.cisa.gov/cisa-tabletop-exercises-
packages.
72 Paul Cichonski et al., NIST Special Publication 800-61r2: Computer Security Incident Handling Guide, NIST (August 2012),
https://nvlpubs.nist.gov/nistpubs/specialpublications/nist.sp.800-61r2.pdf.
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
88Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
that the incident commander should not dive into the technical weeds of the incident, rather keep the
various teams organized and focus on their objectives. Table 12 below describes the teams that may
be involved in resolving a critical security incident and potential breach.
Table 12. Roles and Responsibilities for an Organizational CIRT
Role Responsibilies
Incident
Commander
Individual who will oversee the cybersecurity incident and interact with other
stakeholders in the table.
Executive/Senior
Leadership
An organization’s C-suite or most senior executives. They provide overall direction
and approvals required to resolve signicant cybersecurity breaches. These
individuals should be kept informed throughout the lifecycle of a signicant
cybersecurity incident.
Cybersecurity
Teams
Teams comprised of cybersecurity experts who understand attacks, vulnerabilities,
and the methods by which threat vectors are exploited. They provide technical
knowledge and detail to technical teams and execute procedures in the playbook.
Technical Teams Teams comprising SMEs for the technologies that have been compromised and
who are engaged in developing and implementing the response. These SMEs may
be system owners, system administrators, or other individuals with specialized
IT expertise. They take instruction from the cybersecurity teams as part of the
playbook execution.
Legal Teams Teams comprised of attorneys in your general counsel (internal or external) that help
manage the incident under privilege as well as consult on regulatory expectations.
Emergency
Management
With the potential for cybersecurity incidents to have an operational and patient
safety impact, clinical emergency management function should be connected to
the CIRT. In some organizations the CIRT may take direction from emergency
management, in others it may be reversed. This relationship should be determined
prior to an incident.
Public Affairs/
Marketing and
Communications
Individuals who manage external and internal communications to deliver a
consistent voice and message in the event of a high-visibility cybersecurity incident.
This team is crucial in managing the reputation of your organization.
Privacy and
Compliance
Team
Teams responsible for understanding the full extent of a cybersecurity incident that
involves PHI/PII. This includes conducting a breach assessment for compliance with
federal/state reporting and notication requirements.
Other external
teams
Supporting an incident may require specialized forensics teams, law enforcement,
representatives from CISA or HC3, and other teams to support the investigation and
remediation of the incident.
Consider proactive notication to both CISA and the H-ISAC as part of your IR
playbook. Both notication channels can provide defensive measures to other HPH
organizations based on the context of your security incident. Sharing of IOCs to
either CISA or H-ISAC is protected under the Cybersecurity Act of 2015. Regulators
are not permitted to use any shared information as part of their enforcement actions.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
89Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Security Operations Center Response
The response inside of a SOC is more focused and technical in its nature. The goal of the SOC is to
identify any bad actors that have compromised your organization’s environment and evict them before
wide-spread damage can occur. Typical procedures and processes to consider for the establishment and
running of your SOC are as follows:
• Playbook/Runbook: As mentioned previously, this is a document that contains standard operating
procedures to respond to different types of cyber-attacks. Procedures to respond to a phishing
attack are different from those required to respond to a system intrusion or a ransomware attack.
Each of these attack types is a distinct play in an organization’s cybersecurity playbook. For each
play, it is important to describe the steps that will be followed to mitigate the attack so that your
response is not “made up on the y.” Though each attack has its own unique characteristics and
nuances, your procedures should follow the steps provided in your playbook for that type of attack.
For your reference, a template playbook is provided in Appendix G, Resources and Templates.
Cybersecurity incidents may have a broader organizational impact. Playbooks should tie to
organization-wide emergency management plans (e.g., downtime procedures). It is important to
understand the potential ramication of a cybersecurity incident (e.g., ransomware) may have on
clinical technology and have alignment between the responses. Care should also be taken to ensure
paper documentation (e.g., playbook, phone lists, prescription pads, paper charts) are up to date and
available if a cyber incident has rendered those systems unavailable.
• Tools and technologies: After you establish your policies, CIRTS, and playbook, the next level of
improvement is to congure your tools and technologies to streamline the execution of your plays.
Streamlining connects your IR processes to your security engineering processes to create a continual
feedback loop, which is essential to becoming a resilient organization.
A typical SOC response includes ve key processes:
• Identication: The rst response to any cyber-attack is to understand the scope and extent of
the attack. The identication phase of an attack response involves categorizing and classifying
components of the attack based on your policies and procedures. Critical and sophisticated attacks
warrant a well-organized and effective response.
For example, a general phishing attack that targets a small user set and that is easily identied as
malicious may be assigned a lower level of concern than a targeted phishing attack against a select
user base leveraging the nomenclature of your organization. These highly specialized attacks are
known to be very successful and can easily compromise a user’s credentials or introduce remote-
access malware into your environment.
The identication exercise in a phishing process may be as simple as:
¡ Receiving notication from your user base or through your own detection systems of a phishing
attack or campaign.
¡ Proling and understanding the extent and scope of the phishing attack. Determining its level of
sophistication and intent.
¡ Conducting a basic investigation to determine whether links were clicked, or malware
was delivered.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
90Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Once a potential attack is identied, organizations should connect with their cyber liability insurance
carrier (as required by their policy of insurance). The insurance policy will specify the timeliness and
procedures for notication to qualify as a covered claim. Many insurance carriers designate panels
of service providers that provide services covered under the policy. It is important to use these
panel of forensic rms, legal counsel, or breach notication services to receive the benets under
the insurance policy. Ideally, organizations should identify and establish a relationship with their
preferred vendor from the insurers list of panel providers prior to needing the services.
• Containment: After the extent and scope of the attack is understood, the next step is to contain the
attack before it penetrates further into your organization. This phase is critical and must not be
overlooked; less mature organizations may start xing the vulnerability that was exploited before
they stop the attack. Your playbook should include containment procedures for each play. In some
cases, containment may require shutting down information systems to prevent them from being
compromised if they are vulnerable to the attack.
A containment exercise for a phishing attack may be as simple as the following:
¡ Shunning/preventing any remote access C2 trafc that might be established as part of the attack.
¡ Changing credentials proactively for users who clicked to open a credential-theft
phishing campaign.
• Eradication: This phase of your response focuses your IR effort on eliminating all traces of the attack,
including the attack foothold. This step includes:
¡ Identication of all emails that were delivered to your user base
¡ Removal of these emails from mailboxes of the same user base
¡ Reimaging of endpoints where malicious binaries or malware were downloaded to ensure no
foothold exists
• Recovery: After the threat is neutralized and all malicious activity is removed from your
organization’s systems, you must determine whether to reactivate the compromised technology.
In most cases, the answer to this question will be “of course,” as these technologies fulll a larger
purpose in your organization. In cases where legacy technologies were compromised, however, it
might not be worth the effort and investment to bring them back online.
In either case, the process to restore technical capability in your organization is as important as the
process to remove the threats and malicious activities in your systems. As you restore functionality,
shut down the vectors that made the attack successful. This may be done by patching an exploited
vulnerability or rebuilding an entire system to leverage hardening processes such as those identied
in Cybersecurity Practice #2: Endpoint Protection Systems.
• Lessons Learned/After-Action Report: Arguably, the most important stage of your IR process is a full
debrief with your IR teams after the attack is mitigated and systems are returned to full functionality.
This debrief should prole the successful attack vectors and identify short-term adjustments to
introduce enhanced prevention, detection, or response capabilities, as well as long-term strategic
elements that require more detailed planning.
For example, if your organization falls prey to a sophisticated phishing attack that results in the theft
of multiple credentials, followed by the installation of remote-access tools, a multifaceted set of
mechanisms may be considered for short-term and long-term improvement.
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
91Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Examples may include the following:
¡ Rening a play within the playbook that did not execute as efciently as possible. Timeliness is one
of the most critical aspects of any response; taking too long to ramp up your IR playbook increases
your exposure to a successful attack.
¡ Rening and expanding logging capabilities to detect threats more quickly. Implementing these
capabilities into your SIEMs. Delve into the specic patterns of the attack as much as possible for
lessons learned.
¡ Sharing attack details and information with participating ISACs and ISAOs. This helps other
organizations to prevent validated and vetted threats. It provides greater credence to the
intelligence and increases resiliency of the sector.
¡ Leveraging advanced analytics-based phishing protection tools such as “click protection”
or “attachment sandboxing.” These usually require investment and budget allocation by
your organization.
¡ Refocusing and prioritizing resources to build out greater capabilities to identify and respond
to phishing attacks. From a strategic perspective, it is important to refocus your resources in
response to a threat that is ramping up against your organization.
A feedback loop from your IR processes back into engineering and operations is a key to becoming a
resilient organization. This type of feedback loop enhances an organization’s cybersecurity capabilities
over time and organically, while increasing exibility and agility in IR response processes.
To read an example case of a mock attack, consider the SANS whitepaper “A Practical Example of Incident
Response to a Network Based Attack.”
73
Further details associated with IR playbooks can be found in the
SANS whitepaper, “Incident Handler’s Handbook.”
74
Ransomware-Specic Response
For those specically concerned about ransomware prevention and response, another useful reference
is CISA’s Stop Ransomware website.
75
This site outlines several resources, alerts, and methods for
interfacing with the federal government in event you become a victim to this type of attack. A few
resources to consider on this site include:
• The MS-ISAC Joint Ransomware Guide, which outlines preventative and responsive techniques for
combating ransomware
76
• The CISA Bad Practices, a list of known practices that are considered risky and highly leveraged by
bad actors
77
• A series of training materials for training technical and non-technical users
• A series of freely available services provided by CISA to protect critical infrastructure, such as
phishing simulations, vulnerability assessments, and penetration assessments
73 Gordon Fraser, “A Practical Example of Incident Response to a Network Based Attack,” The SANS Institute (August 16,
2017), https://www.sans.org/white-papers/37920/.
74 Patrick Kral, “The Incident Handlers Handbook,” The SANS Institute. February 21, 2012 https://www.sans.org/white-
papers/33901/.
75 StopRansomware.gov, CISA (Accessed May 31, 2022), https://www.cisa.gov/stopransomware.
76 “Ransomware Guide,” MS-ISAC and CISA (September 2020), https://www.cisa.gov/sites/default/les/publications/
CISA_MS-ISAC_Ransomware%20Guide_S508C.pdf.
77 “Bad Practices,” CISA (Accessed June 2, 2022), https://www.cisa.gov/BadPractices.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
92Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
It is highly recommended to contact the FBI or CISA if you have been a victim of a ransomware
attack. The FBI and CISA both recommend strongly against paying any ransoms, as ransom payments
continue to fund the bad actors and criminal enterprises. If your organization decides to pay the ransom,
although extremely discouraged, it is highly advisable to do so under the guidance of CISA, the FBI, and/
or legal counsel. As this is an ever-evolving situation, you will want to ensure you have the proper legal
authorizations in place if a payment is deemed necessary.
Contact the local FBI ofce closest to you.
78
Contact CISA directly at: [email protected] or (888) 282-0870.
8.M.C: Information Sharing and ISACs/ISAOs
NIST Framework Ref: ID.RA-2
Security engineering and operations activities tend to focus on preventing cyber-attacks and building
out systems that enable streamlined execution of IR functions. However, not all attacks are equal. Some
are perpetrated by “script kiddies,” relatively unskilled individuals who use crude scripts and programs
to attempt to exploit whatever organization they can. Some threat actors are highly competent
hackers backed by substantial resources and a strong desire to gain entry to your specic organization.
Differentiating these types of attacks falls under the discipline of threat intelligence.
By banding together with peer organizations, ISACs and ISAOs establish and maintain channels for
sharing cyber intelligence. The means to share this intelligence vary in sophistication; most mature ISACs
leverage common standards and formats, such as STIX and TAXII, as well as ash reports that prole
current attacks. ISAC or ISAO participation offers substantial value to an organization. It connects your
cybersecurity professionals with the greater cybersecurity community.
As with all disciplines, there are multiple levels of maturity within the threat intelligence discipline. The
most basic sharing of threat intelligence involves consuming lists of “vetted bad IP addresses” or “feeds”
from commodity sources. These sources have been well curated to identify where the loudest and most
obvious attack space resides. Organizations can use multiple means to consume these feeds, but the most
usual process is to subscribe to a daily download of IOCs.
Health-ISAC (H-ISAC)
The largest ISAC for the Health and Public Health Industry is H-ISAC. H-ISAC is a member driven
organization that offers an array of cyber threat intelligence and hygiene services.
79
Members share
threat intelligence, IOCs and TTPs in both an automated and manual method. Your organization also
produces advisories for the whole HPH sector, regardless of membership, as well as more specialized
analysis provided to members. H-ISAC is connected to other sectors’ ISACs as well as maintains
information sharing protocols with the federal government.
78 “Field Ofces,” FBI (Accessed May 31, 2022), https://www.fbi.gov/contact-us/eld-ofces.
79 Health-ISAC (H-ISAC), https://h-isac.org/.
Cybersecurity Pracce #8: Security Operaons Center and Incident Response
93Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Other ISAOs and ISACs
Members of the HPH Sector can join other ISACs or get involved in smaller ISAOs. The Population Health
ISAC (PH-ISAC) is a member driven organization and focuses on community health centers, behavior
health, rural and community hospitals and provides proactive services for these systems.
80
The IT-ISAC
focuses on all IT cross sector. Other organizations can create their own ISAOs, the terms of which are
dictated under the ISAO Standard Organization.
81
CISA Cyber Hygiene Services
CISA also provides a wide variety of free services to Critical Infrastructure, referred to as “CyHy.”
82
The
services available are as follows:
• Vulnerability Scanning: Evaluates external network presence by executing continuous scans of public,
static IPs for accessible services and vulnerabilities. This service provides weekly vulnerability
reports and ad-hoc alerts.
• Web Application Scanning: Evaluates known and discovered publicly accessible websites for
potential bugs and weak conguration to provide recommendations for mitigating web application
security risks.
• Phishing Campaign Assessment: Provides an opportunity for determining the potential susceptibility
of personnel to phishing attacks. This is a practical exercise intended to support and measure the
effectiveness of security awareness training.
• Remote Penetration Test: Simulates the tactics and techniques of real-world adversaries to identify
and validate exploitable pathways. This service is ideal for testing perimeter defenses, the security of
externally available applications, and the potential for exploitation of open-source information.
To request any of these services, send an email to vulner[email protected] with the subject line of
“Requesting Cyber Hygiene Services.”
Sub-Practices for Large Organizations
8.L.A: Advanced Security Operations Center
NIST Framework Ref: N/A
In addition to the basic SOC practices already discussed, an organization’s move to more advanced
security management should include expanding its SOC to be staffed and monitored 24 hours per day,
7 days per week, 365 days per year (24x7x365). This is strongly recommended for medium and large
organizations, given that cybersecurity incidents may happen any time of day. Delays between the initial
incident and response may result in a worse outcome.
The models described below can account be used in whole or part, based on the types of technologies
and processes running within your SOC. For example, some organizations might elect to outsource
Tier 1 playbook monitoring of their SIEM and EDR tools but keep Tier 2 escalations in-house. Other
80 “CommHIT Information Sharing & Analysis Centers (ISACs),” CommunityHealth IT (Accessed May 31, 2022), https://
www.communityhealthit.org/isacs/.
81 ISAO Standards Organization, https://www.isao.org/.
82 “Cyber Hygiene Services,” CISA (Accessed June 2, 2022), https://www.cisa.gov/cyber-hygiene-services.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
94Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
organizations might elect to keep all SIEM management in-house but elect to use EDR monitoring in an
outsourced manner. The models selected should be based on the best risk management and nancial
model for your organization. There are multiple methods to achieve this model, all of which have benets
and constraints. Some of these methods are described below:
• Fully outsourced: All SOC and threat actions are outsourced to a third-party provider who has the
required infrastructure, staff, and capabilities. Such providers normally install sensors on your
networks and use them to collect necessary log information that enriches detection and response
activities. SOC analysts actively look for threats and provide your internal IR personnel with specic
actions to take when threats are identied.
This model has the advantage of scale and capability. It is difcult to hire and retain qualied security
analysts to provide this dedicated function. Additionally, organizations benet from the shared
intelligence discovered by the service provider’s other clients. The main disadvantage from the use
of analysts supplied through third-party vendors is that they often do not fully complete response
actions. Your internal teams must be available to provide follow-up engagement. Furthermore,
cybersecurity tool investments made by your organization might not be fully leveraged, as third-
party service providers are likely to use their own tools.
• Fully insourced: All SOC and threat actions are handled with internal staff and infrastructure. This
model requires the buildout of a dedicated physical space with the IT infrastructure and tools
necessary to support your IR personnel. It requires a combination of skills from security engineers,
incident handlers, and threat hunters.
This model has the advantage of situational awareness and an in-depth understanding of your
organization’s business requirements and nuances. Internal staff are accustomed to the specic
needs of your organization. Additionally, internal staff understand the context of an organization’s
various systems in far more depth than an outside service provider could. The main disadvantages
of this model relate to cost, workforce retention, and threat intelligence. Building out an internal
SOC can be costly if your organization lacks existing facilities to support it. Moving to a 24x7x365
operation requires hiring new employees and supervisors to ensure effective management and
coverage during holidays and time off. With this model, your organization does not necessarily get
current information about threat actions occurring in other organizations. Consider leveraging
student workers/internships to staff a fully insourced SOC. This model has been outlined within
HSCC’s Health Industry Cybersecurity Workforce Guide.
83
• Hybrid: The SOC and incident handling functionalities attempt to take advantage of the strengths
of the outsourced and the insourced models while minimizing the disadvantages of each. In the
hybrid model, organizations contract with a service provider who provides 24x7x365 monitoring and
response by remotely accessing your organization’s existing security technologies (e.g., SIEMs, IPS,
rewalls). The service provider provides facilities and staff for monitoring and response actions, and
your organization provides the tools and escalation processes.
The hybrid model tends to offer exibility and scaling of existing investments made in cybersecurity
technologies, processes, and people. However, it requires specic and scripted procedure playbooks
(developed by your organization) to be effective. It is up to the contracting organization to ensure
that their service provider has implemented and is performing to the specications set by the
83 Healthcare Industry Cybersecurity Workforce Guide: Recruiting and Retaining Skilled Cybersecurity Talent, Healthcare &
Public Health Sector Coordinating Council (HSCC) (June 2019), https://healthsectorcouncil.org/workforce-guide/.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
95Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
established procedures. Lastly, in this model, organizations lose some of the situational awareness
normally provided by internal handlers. Precise roles and responsibilities must be established to
achieve the desired outcome.
8.L.B: Advanced Information Sharing
NIST Framework Ref: ID.RA-2
Leveraging threat intelligence can be challenging. Your organization must establish a threat model, ingest
data according to the model, and automate data collection and response. This requires dedicated human
and technology resources to be successful.
MITRE has developed a model to manage threats. “Adversarial Tactics, Techniques, and Common
Knowledge (ATT&CK™)” is a curated knowledge base and model for cyber adversary behavior. It
addresses the phases of an adversary’s lifecycle and the platforms that are targeted. ATT&CK is useful
for understanding security risks from known adversary behavior, planning security improvements,
and verifying that defenses work as expected.
84
It is recommended that organizations consider
using this model in addition to STIX and TAXII automation methods to build out a robust threat
intelligence program.
Intelligence gathering organizations or departments within organizations, including some ISACs/ISAOs,
have a vested interest in getting “deep intelligence” directly from the attacker community. This capability
requires substantial investment and specialized talent (e.g., intelligence ofcers), so this level of maturity
is not achievable in most large organizations. However, with proper investigation, the fruits of intelligence
organizations’ labor can benet the HPH sector immensely.
For a review of Healthcare specic sharing organizations consider reviewing HSCC’s Health Industry
Cybersecurity – Matrix of Information Sharing Organizations (HIC-MISO).
85
8.L.C: Incident Response Orchestration
NIST Framework Ref: PR.IP-9
Many specialized tools exist to provide organizational cybersecurity. It can become complicated to
leverage all these tools at once. Examples include SIEMs, user behavior analytics, deception technologies,
email protection platforms, and EDR technologies. Though tools like SIEMs are designed to ingest
information from multiple sources and provide context, this capability is dependent on the extensibility of
log data, as well as the workow and process capabilities of the SIEM technology.
SIEMs are good at developing alerts and notifying security resources about emergent issues, but they
are generally not as robust in their execution of IR playbooks. This is where IR orchestration tools come
in handy. When playbooks have been created and approved, IR orchestration tools ensure that playbook
execution is consistent. Without IR orchestration, cybersecurity personnel must manage IR consistency.
IR orchestration tools enable cybersecurity personnel to focus on the incident, rather than on the
consistent execution and documentation of a response play.
84 MITRE ATT&CK®, https://attack.mitre.org/.
85 “Health Industry Cybersecurity — Matrix of Information Sharing Organizations (HIC-MISO),” HSCC (Accessed May 31,
2022), https://healthsectorcouncil.org/hic-miso/.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
96Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
In addition to monitoring workow, IR orchestration tools can pull data from system security stacks and
present it to the incident responder in a centralized dashboard. Examples of data that may be pulled into
this dashboard include: SIEM, log data, Dynamic Host Conguration Protocol logs, asset inventories, anti-
malware consoles, vulnerability management data, threat intelligence information, identity management
systems, and endpoint security technologies. Each data type provides a unique perspective on the threat
that your organization is experiencing.
8.L.D: Baseline Network Trafc
NIST Framework Ref: ID.AM-3 / DE.AE-1
The network baseline is dened as a set of metrics that describe normal operating parameters. Setting
the baseline enables engineers to catch changes in trafc that could indicate an application performance
problem or a security breach. It also makes the “before” and “after” when a change is made clear, making
it easier to measure the benet and calculate a return on investment (ROI). Without an accurate baseline,
any kind of measurement being done is basically a best guess. This can be done manually, or you can
invest in technologies that can automate the process.
Taking baseline readings for your network trafc is the rst step to efciently spotting potentially
fraudulent activity. Regularly monitoring network trafc will allow you to:
• Understand healthy network patterns and trafc trends.
• Evaluate network management policies compliance.
• Understand how the network resources are allocated.
• Accelerate to troubleshoot network issues (i.e., abnormal trafc and spam trafc, etc.).
• Provide data on network and security management to support decision making.
• Provide history statistics on network upgrade.
Understanding Network Performance
• Device availability: Monitor all network device availability, particularly the critical servers on your
network. If an important network device such as a central server goes down, it can take down your
entire network (or a signicant part of it) along with it.
• Storage: Keep an eye on the storage capacity and disk space on all your critical servers. If your
storage systems are getting too full, this can cause slowdowns and problems for your end users.
Additionally, assuming you have good knowledge of what your storage systems parameters are, you
will be better able to detect anomalous behavior.
• Security: Make sure your rewalls, AV and malware protection, and update servers are functioning
and congured correctly.
• Trafc: Monitor all trafc coming in and out of the network. This will help you to establish clear
baselines and identify peak periods in advance, so you can undertake appropriate capacity planning
to mitigate times when large amounts of trafc are coming through.

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
97Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Monitoring Unusual Network Activity
Regarding the role of baselines in network security, if there is a huge spike in trafc, that could indicate
some kind of volumetric denial of service (DoS) attack. But baselines can do more than that. Consider an
instance where a certain user’s normal trafc patterns indicate the network is being used to access the
customer relationship management (CRM) system, email, and internet. Then, suddenly, there is trafc
going from the user’s computer to the accounting server. This could indicate that the computer was
hacked, and malware is attempting to access and compromise nancial information. Any kind of trafc
that deviates too far from the norm should lead to the quarantining of an endpoint. This can help mitigate
risk and minimize the damage when a breach occurs. Similarly, if the accounting system was connecting to
unknown sites on the internet, it could indicate malware is present on the server.
Consider these techniques to monitor unusual network activity:
• Compile the list of known administrative tools leveraged by your organization for remote administration.
These tools will be installed on endpoints. Allowlist the use of those tools and then congure
your EDR technologies to ag on the use of any new administrative technology that has not been
previously used. (These administrative tools are not inherently malicious but could be used for
malicious purposes).
• Determine the user accounts that are authorized to make administrative changes in the production
environment. Allowlist those accounts for these purposes. Key on any other administrative accounts
not congured in that allowlist and investigate their use. This could catch a user account that has
been granted elevated privileges by a bad actor and used in a malicious manner.
Measuring Network Changes
Baselines also help measure the impact of architectural changes. For example, if a company is using a
traditional Multiprotocol Label Switching (MPLS) network, it can set baselines to understand the volume
of trafc owing over the WAN links. The baseline can then be used to help the business understand
whether they are spending the right amount on the network or overspending.
8.L.E: User Behavior Analytics
NIST Framework Ref: PR.PT-1 / DE.AE-1
One technique to make a SIEM more effective is leveraging User and Entity Behavior Analytics (UEBA).
UEBA solutions look at patterns of human behavior, and then apply algorithms and statistical analysis to
detect meaningful anomalies from those patterns—anomalies that indicate potential threats. Increasingly
this analysis is performed with machine learning and articial intelligence (AI) algorithms that reduce
false positives and identify potential incidents a human would not easily see. Instead of tracking devices
or security events, UEBA tracks a system’s users (whether it is the authorized individual or a threat actor
who has compromised a valid account) and its devices. Although attackers can generate new accounts for
access attempts, they are aware that most organizations monitor systems for new accounts, especially
those with privileged access. The exploitation of existing accounts, however, might go unnoticed without
a UEBA system in-place.
Access logs within applications like Electronic Health Record (EHR)/EMR provide a rich source of data
for such UEBA. Many certied EHR/EMRs are required to create comprehensive logs but do not alert on
suspicious behavior or perform trend analysis. These applications generate substantial volumes of access

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
98Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
logs that are often overlooked for analysis. If used proactively, they can be very useful with identifying
potential insider issues.
UEBA can address a variety of use cases. The most common include inappropriate access to information
(e.g., downloading an unusual number of records), account compromise, privilege account abuse,
anomalous network trafc, and data exltration. To create actionable alerts, the UEBAs system creates
a prole of baseline user and endpoint activity throughout your organization’s digital ecosystem. The
tool ingests the most relevant user activity logs from these systems as well as existing authentication
and authorization systems and can also monitor network trafc. Activity that deviates from the user
prole create alerts to system analysts or administrators or endpoint enabling IR actions to be executed
according to the proper playbooks.
8.L.F: Deception Technologies
NIST Framework Ref: N/A
Deception technologies expand on the honeypot and honeynet techniques of old, scaling them for larger
enterprises. These techniques place “fake systems” (a.k.a. honeypots) or “fake breadcrumbs” (a.k.a.
honeytokens) throughout the digital ecosystem and wait for them to be “tripped.” They work on the
principle that communications should not occur in a system that serves no purpose in your organization.
Deception technologies discover attackers who have placed a foothold in your organization’s network
and are attempting to pivot to nd targets of interest. These targets may be simple (e.g., le storage
systems, email systems) or they may be complicated (e.g., EMR or imaging systems). In all cases, the
goal of the attacker is to leverage access already obtained to steal data, conduct an extortion attack (i.e.,
ransomware), or other malecence.
The log les of these systems should be interfaced with your organization’s SOC, as dened within 8.M.A:
Security Operations Center (SOC). If such communication occurs, it should be brought to the attention of
the IR teams for further investigation.
Some common techniques for implementing deception technologies include:
• Server-based honeypot: Server based honeypots are designed to mimic real servers. Ideally, they will
be deployed to look like known servers in your environment, such as a le server, domain controller,
web server or even middleware systems. To implement in this manner, conduct port scans against
your known production, test, development, or sandbox systems and congure the honeypots to
mimic the services and service version levels. Deploy these systems either nearby, or in network
zones where it is known that they do not serve a production value.
• Registry-based honeytokens: A registry-based honeytoken can be placed within the Windows registry
nearby other target rich registry keys, such as password hashes, software installations or other
registry hive information. A popular technique is to create a ctious password-hash that, if detected
through use of EDR or extended detection and response (XDR) tools, could indicate the compromise
of an endpoint.
• Account-based honeytokens: As with registry-based tokens, one can create an enterprise account that
has no privileges in the environment. If that account is ever used for logins or other authentication
measures, it would be indicative of a further compromise inside of the environment. A common

Cybersecurity Pracce #8: Security Operaons Center and Incident Response
99Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
technique there is to establish a weak password without expiration, making this a “lure” for bad
actors to attempt to compromise.
• Fake Patient Data: Another popular technique is to create a fake patient within an EMR, enterprise
data warehouse (EDW), or other data repositories. At this point, you can congure your DLP systems
to key off this fake information and signal critical alerts if it is ever transported inside or outside of
your organization.
Playbooks should be established for each of these dened implementations above and run through
the SOC. In all cases, it is recommended to pivot off the activity of a honeypot or honeytoken and use
that to prole the bad actor and determine their specic IOCs. These could be direct remote access
channels, command and control trafc, user accounts, and le hashes of interest. Once the IOCs have
been determined, you can evict the bad actor from your environment and continue to monitor for more
intrusive behavior.
Key Mitigated Threats
1. Social engineering
2. Loss or theft of equipment
3. Insider, accidental or malicious data loss
4. Attacks against network connected medical devices that may affect patient safety
Suggested Metrics
• Time to detect and respond in aggregate, measured weekly. The goal is that an IR protocol should kick
off within X hours after detection of an incident, and the incident should be mitigated within Y hours
after response. Lag time between occurrence and detection of a security incident should be fewer
than Z days.
• Number of true positive incidents executed by incident category, measured weekly. Though there is
no specic goal for this metric, it is important to monitor trends in incidents that occur in your
organization. This will inform the larger security strategy over time based on actual threats in
your organization.
• Number of backup failures, measured weekly. The goal is to minimize the number of backup jobs that
fail and to provide continual assurance that backup jobs are executing as intended.
• Number of notable (or critical- and high-rated) security incidents, measured weekly. This will provide
a proled enumeration of each incident. Each response to a notable security incident should
be executed consistently and thoroughly. Each incident should have an after-action report.
The goal is to demonstrate that after-action reports and incident reports are written for each
notable security incident. This will help with the development and implementation of continual
improvement processes.
100Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Areas of Impact
PHI
Medium Sub-Practices
9.M.A Asset Management
9.M.B Endpoint Protections
9.M.C Identity and Access
Management
9.M.D Network Management
9.M.E Vulnerability
Management
9.M.F Contacting the FDA
Large Sub-Practices
9.L.A Security Operations and
Incident Response
9.L.B Procurement and
Security Evaluations
Key Threats Addressed
• Attacks against network
connected medical devices
that can affect patient safety
405(d) Resources
• Prescription Poster:
Network Connected
Medical Devices
Cybersecurity Pracce #9:
Network Connected Medical
Devices
Healthcare systems use many diagnostic and therapeutic methods
for patient treatment. These range from technological systems that
capture, render, and provide detailed images of scans to devices
that connect directly to the patient for diagnostic or therapeutic
purposes. Medical devices range from straightforward monitors,
such as bedside monitors that measure vital life-sustaining activity
to sophisticated multi-function machines, like infusion pumps that
deliver specialized therapies and require continual drug library
updates. Network connected medical devices are network-based
devices that leverage networking protocols to communicate and
transmit clinical information, such as Bluetooth, TCP/IP and other
networks-based devices. These complex devices create and maintain
copious amounts of data that affect patient safety, well-being, and
privacy. Their interconnection with information systems that manage
clinical decision making represent potential attack vectors in HDOs’
digital systems. As such, these devices should be robustly designed
and properly secured.
This section focuses on the methods that HDOs can employ to
protect network connected medical devices. Specically, it addresses
the actions that HDOs are permitted to take, how to align with the Medical Device and Health IT Joint
Security Plan, and how to best work with device manufacturers and the FDA.
The creation and deployment of network connected medical devices has rapidly expanded in the past few
years. These online medical devices have become increasingly attractive to cybercriminals. Each device
may contain hardware, software, and/or sensors that gather, store, and transmit healthcare data and
condential patient information over health system’s clinical network and internet.
Many IoT devices interact with the physical world in ways conventional IT devices usually do not. The
potential impact of some IoT devices making changes to physical systems and thus affecting the physical
world needs to be explicitly recognized and addressed from cybersecurity and privacy perspectives. Also,
operational requirements for performance, reliability, resilience, and safety may be at odds with common
cybersecurity and privacy practices for conventional IT devices.
Additionally, some medical devices may only be intermittently connected to the network, or have yet
to be onboarded. The problem is that these devices might still be at risk from vulnerbailities, thus it is
recommended that these vulnerabilities be corrected or mitigated before being attached to the network.
There is also the possibility of “rogue” medical devices getting connected to the network. These devices
may be used by the healthcare provider team as part of an assessment or vendor trial or demo.

Cybersecurity Pracce #9: Network Connected Medical Devices
101Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
How to Prevent Spread of Security Impacts
There are four high-level goals to mitigate cybersecurity and privacy risks for IoT devices:
1. Protect Patient Safety and Device Effectiveness: Patients who are receiving care from network
connected medical devices are at risk of adverse events resulting from device vulnerabilities being
exploited that impact device availability and performance. Security controls internal and external to
the device aim to assure the safety and effectiveness of the device.
2. Protect Device Security: Prevent a device from being used to conduct attacks, including participating
in distributed denial of service (DDoS) attacks against other organizations, and eavesdropping on
network trafc or compromising other devices on the same network segment. This goal applies to all
IoT devices found on the network.
3. Protect Data Security: Protect the condentiality, integrity, and/or availability of data (including PII and
PHI) collected by, stored on, processed by, or transmitted to or from the connected medical device.
This goal applies to each IoT device except those without any data that needs protection.
4. Protect Patient Privacy: Individuals’ privacy can be impacted by the authorized processes surrounding
PII/PHI. This goal applies to all network connected medical devices that process PII/PHI or that
directly or indirectly impact individuals.
Why do medical devices create unique challenges?
Condentiality, integrity, and availability of patient data are paramount, and still breaches occur almost
daily in healthcare. While impacting data is devastating to the patient and provider, compromised
network connected medical device integrity can be catastrophic. Emergency room doctors rely heavily
on a computed technology (CT) scanner’s availability and integrity to quickly diagnose stroke patients and
determine if a stroke is hemorrhagic or ischemic. Delayed care or misdiagnosis due to a compromised CT
scanner could easily result in loss of motor functions, brain damage, or even death.
Many network connected medical devices interact with the physical world in ways conventional IT devices
do not. Infusion pumps regulate the delivery of life-sustaining medication. Implanted cardioverter
debrillators deliver electrical shocks and restore the heart to normal rhythms. Hackers have
demonstrated vulnerabilities in these types of devices which allow increasing dosages or manipulating
shocks that result in sudden death. While these examples are extreme, it is clear that interfering with the
stated performance of network connected medical devices negatively impacts the quality of patient care
and increases the nancial risk to the provider.
Traditional IT devices like workstations, servers and routers have been designed with security in mind
so can be fully integrated and managed by traditional information security tools. Most medical devices,
facilities management devices and some IoT devices do not share this same design and therefore create
challenges for IT and Security teams.
• Visibility, Inventory & Device Scanning: The volume of medical devices ranges from 5-14 devices per
bed, which creates an exponentially complex challenge for creating, maintaining and monitoring a
growing, changing and mobile inventory. Network device scanning tools are considered invasive
or active. These tools interact with the network device to obtain granular detail about the device.
The ability to identify a computer’s make, model, operating system, IP address, serial number,
MAC address, etc. is standard for traditional devices. This level of detail allows traditional security
tools to make determinations regarding risk levels and vulnerabilities, mitigations or remediations.

Cybersecurity Pracce #9: Network Connected Medical Devices
102Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Medical devices are not designed to support active scanning. Active scanning can interfere with
the performance of a medical device, which could be attached to a patient. Disrupting normal
functionality or “knocking the device over” could negatively impact patient care. Identifying the
medical devices on your network and gleaning the granularity of detail on each device required to
make intelligent cybersecurity decisions had been a challenge for healthcare IT and Security teams.
• Passive Scanning & Communication Protocols: An optional technique for device identication is
passive scanning. Like active scanning, traditional IT-based passive scanning tools can read the
packets of information traveling across the network and make determinations. This becomes a
challenge because traditional IT devices communicate in protocols like TCP/IP, HL7 and DICOM
and traditional security tools are limited to understanding (reading packet information) written in
these protocols. Medical devices, facilities devices and many IoT devices communication in unique
protocols. Once again, creating a challenge in the rudimentary step of identifying what devices are
on the network.
• Medical Device Risk Management: How can your organization determine the device vulnerabilities,
the environmental risk posed by or to the device, the device risk level and appropriate controls
required to reduce risk safely and effectively if your organization has no visibility on the devices and
their details?
• Device Monitoring & Network Policy Management: NAC systems are commonly used to manage
traditional endpoint devices: servers, desktops, laptops, and portables. NAC can manage traditional
network endpoints because they have visibility on these devices. However, most NACs have
inadequate contextual information about medical device use, trafc ows or operational status.
There are two main challenges with network policy management:
¡ Determining Policies: Without accurate identication of the device and a full understanding of the
other network devices it is communicating with, creating network communication restriction on
medical devices, potentially providing life-saving care, requires a tremendously labor-intensive
effort in mapping. Therefore, many network policies have little or no restrictions on these devices
and they are simply put in an unrestricted VLAN with other unknown devices with unknown risks.
¡ Operationalization: When network communication policies can be identied, converting those
logical communication restrictions into the network software is also labor-intensive. Programming
and testing restrictions are critical to maintain and protect clinical device performance.
• Legacy Devices: These are dened as a device that cannot be reasonably protect against current
cybersecurity threats.
86
Traditional IT device lifecycles are two to four years. Medical device
lifecycles can extend beyond 15 years. Clinical Engineering departments work hard to maintain and
extend the life of devices. But most health organizations utilize the devices beyond the EOS for the
operating systems and other components within the device. Management of legacy technologies in
healthcare is a multi-faceted challenge. Although the functional or maintenance obsolescence, or
even device safety risks because of device EOS, are not new problems, the inclusion of cybersecurity
considerations heightens the frequency of such events and increases the urgency of addressing them.
86 “Principles and Practices for Medical Device Cybersecurity,” IMDRF Medical Device Cybersecurity Working Group
(March 2020), https://www.imdrf.org/sites/default/les/docs/imdrf/nal/technical/imdrf-tech-200318-pp-mdc-n60.
pdf.
Cybersecurity Pracce #9: Network Connected Medical Devices
103Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Remote Access: Manufacturers may need to access the medical devices remotely over the network
for updates or to mitigate vulnerabilities. This functionality is built into the device which causes
challenges in monitoring communications, managing access, and determining restrictions. Leveraging
a device’s remote access capabilities is a primary vector for bad actors to enter the network.
• Risk Analysis & Electronic Public Health Information (ePHI): The HIPAA Security Rule requires an
accurate and thorough assessment of the potential risks and vulnerabilities to the condentiality,
integrity, and availability of ePHI held by the covered entity or business associate. While MDS
2
forms
can identify which devices have ePHI, it is a static variable that is not being identied within the
context of network communication. How are organizations determining if data stored or transmitted
by medical devices is encrypted? The volume of devices combined with the complexity of identifying
ePHI on the network is compounded when factoring in the risk of the device. All of which is required
under the HIPAA Security Rule for compliance.
¡ NIST SP 800-66r2 ipd Implementing the Health Insurance Portability and Accountability
Act states:
87
Prepare for the Assessment: Before beginning the risk assessment, the regulated entity should
understand where ePHI is created, received, maintained, processed, or transmitted. Identify where
ePHI is generated within your organization, where and how it enters your organization (e.g., web
portals), where it moves and ows within your organization (e.g., to specic information systems),
where it is stored, and where ePHI leaves your organization. Is ePHI transmitted to external third-
parties, such as cloud service providers or other service providers? The scope of a risk assessment
should include both the physical boundaries of a regulated entity’s location and a logical boundary
that covers any devices or media that contain ePHI, including electronic networks through which
ePHI is transmitted, regardless of its location.
• High Knowledge/Limited Resources: Cybersecurity for medical devices creates new complexities
related to personnel resources and departmental alignments. Clinical Engineering is responsible
for the devices and often the only individuals licensed to repair/congure them under compliance
requirements. The IT and Security teams are versed in risk mitigation and how the device operates
on the network. These departments will need to work more collaboratively, and some organizations
have created new positions that focus on spanning the Cybersecurity for Medical Device channel.
But medical device cybersecurity risk management is evolving. Progressive HDOs are increasing
collaboration, implementing a device security plan, exploring leading-edge solutions, and leveraging
additional resources to bring the healthcare sector into the 21st century.
Asset Discovery and Security (ADS) monitoring solutions can automate many of the tasks surrounding
the implementation of controls, additionally they can collect device specic and network ecosystem data.
Sophisticated and health industry specic deep packet inspection, combined with machine learning and
AI based systems, can classify and prole all medical devices on the network. While an ADS can automate
discovery, monitoring, analysis, and onboarding of devices, integration with a Computerized Maintenance
Management Systems (CMMS)/Conguration Management Database (CMDB) can operationalize
87 NIST Special Publication NIST SP 800-66r2 ipd Implementing the Health Insurance Portability and Accountability Act (HIPAA)
Security Rule: A Cybersecurity Resource Guide, NIST (July 2022), https://nvlpubs.nist.gov/nistpubs/SpecialPublications/
NIST.SP.800-66r2.ipd.pdf.
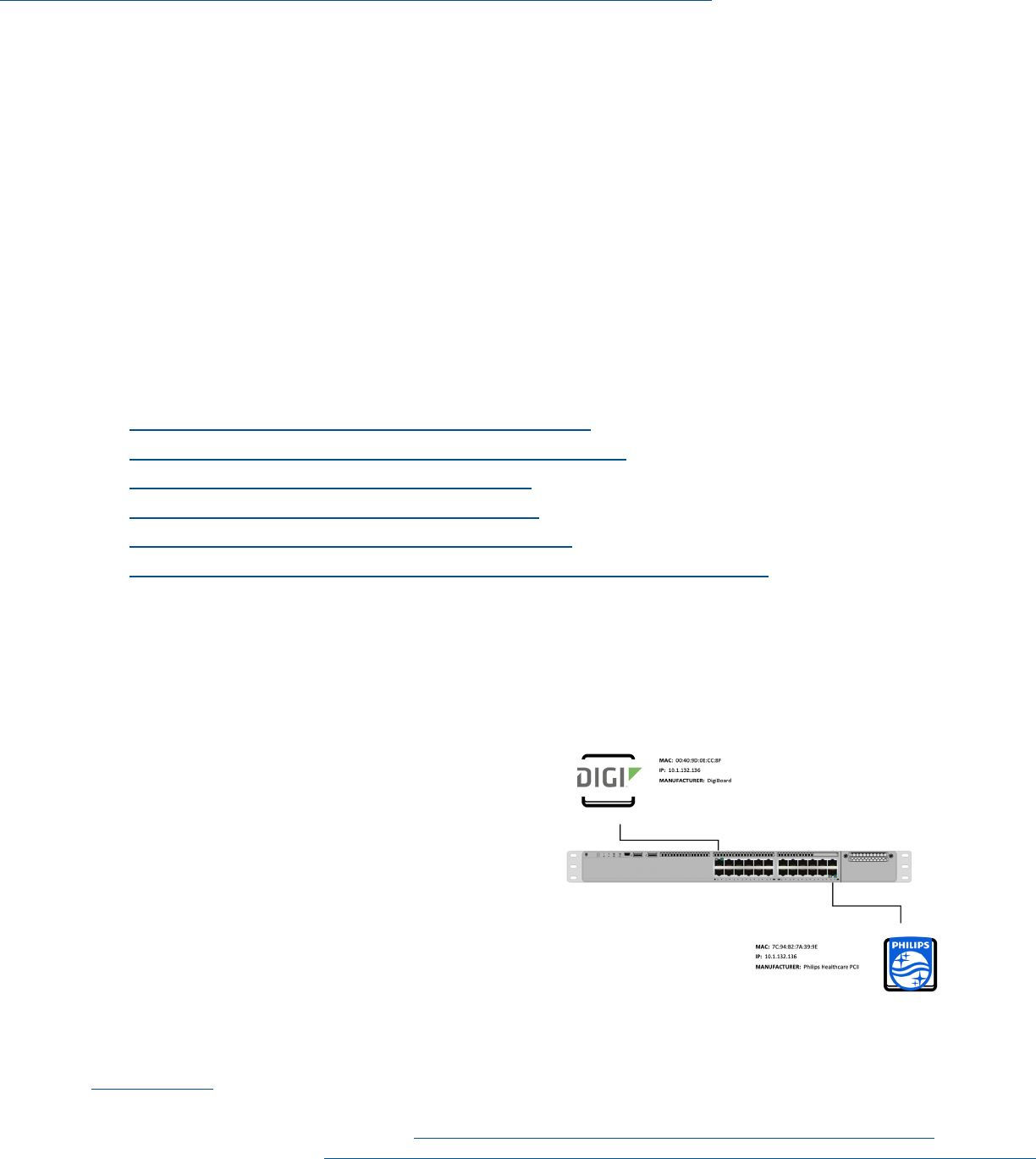
Cybersecurity Pracce #9: Network Connected Medical Devices
104Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
maintenance and remediation workows, and coordinate security orchestration and incident response.
Together, both tools create an efcient, effective, and scalable solution.
Given the highly regulated nature of medical devices and the specialized skills required to modify
them, HDOs should take great care in making conguration changes without utilizing technical support
documentation or service programs endorsed by the device manufacturer. Doing so may put the HDO
at risk of voiding warranties, resulting in legal liability, or at worst, harm to the patient. Therefore,
traditional security methods used to secure assets should be carefully reviewed prior to being deployed
or applied to medical devices. For example, one cannot simply apply a patch to a vulnerable component
of the operating system that runs a medical device without fully assessing the impact on the operation or
capabilities of the medical device.
Medical Device Management
Medical devices that can connect to the internet are a specialized type of IoT device, specic to providing
clinical diagnosis or treatment within HDOs. Nevertheless, cybersecurity for medical devices requires
many of the cybersecurity practices already discussed in this document:
• Cybersecurity Practice #2: Endpoint Protection Systems
• Cybersecurity Practice #3: Identity and Access Management
• Cybersecurity Practice #5: IT Asset Management
• Cybersecurity Practice #6: Network Management
• Cybersecurity Practice #7: Vulnerability Management
• Cybersecurity Practice #8: Security Operations Center and Incident Response
Rather than recreating these cybersecurity practices, HDOs are encouraged to extend the relevant
cybersecurity practice from each section, implementing it appropriately for medical device management.
The following sections expand on how the practices listed above apply in the specialized case of
medical devices.
Medical devices typically connect to larger
information systems or applications. For example,
a CT scanner may connect to a picture archiving
and communication system (PACS), which, in
turn, is connected to specialized image-reading
workstations.
88
In such environments, the practices
listed below are important, not only for the medical
device itself (in the case the CT scanner), but also
for the larger information systems and connected
endpoints. Consider all these safeguards,
as applicable.
88 NIST Special Publication 1800-24: Securing Picture Archiving and Communication Systems (PACS): Cybersecurity for the
Healthcare Sector, NIST (December 2020), https://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.1800-24.pdf.
Figure 3. Last Generation
Technology—Limited Viability

Cybersecurity Pracce #9: Network Connected Medical Devices
105Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Medium-
Sized Organizations
9.M.A: Asset Management
NIST Framework Ref: ID.AM, ID.AM-1, PR.IP-6
When feasible, medical devices should have the
following controls enabled:
• Inventory, hardware: All medical devices should
be added to an inventory that can reect the
core components of the devices themselves.
You may use your general ITAM inventory, as described in Cybersecurity Practice #5: IT Asset
Management. Alternatively, you may need to employ specialized tools designed specically for
tracking the lifecycle of medical devices. Such systems can be useful for maintaining preventative
maintenance schedules.
• Inventory, software: Implement a software component inventory for your medical devices.
Manufacturers should be able to deliver to the HDO a full listing of software components
(including operating systems and software application components developed by vendors, as well
as components licensed from third-parties), with at least major version information. Such lists are
sometimes referred to as “bills of materials.” Information about software components should be
maintained in a scalable database managed by the HDO and updated as part of the standard device
management practices.
• Wiping: When a medical device is slated for decommissioning, it is crucial to ensure that all data on
the device are wiped. Typically, these devices are returned to the vendor and potentially resold or
delivered to other organizations for destruction. Federal and state requirements for the protection
and disposal of hardware and media that contain PII prohibit the allowing the data to be accessed by
these other parties.
Within the medical technology discipline, it is recommended to store the results of these inventories into
CMMS. These systems are like ITAM systems for IT assets but contain specialized elds for the tracking
of maintenance, recalls, and other key attributes specic to medical devices.
Automated Asset Discovery
It is common for an HDO to have hundreds to thousands of medical devices deployed throughout the
system. As such, conducting these hardware and software inventories manually is likely to be inefcient.
Automated tools, called ADS monitoring systems, exist to assist with this issue. These ADS tools can
automate many control implementation tasks while collecting device specic and network ecosystem
data. Sophisticated machine learning and AI based systems can classify and prole all medical devices on
the network.
While an ADS can automate discovery, monitoring, analysis, and onboarding of devices, integration with a
CMMS to operationalize maintenance and remediation workows, and coordinate security orchestration
and IR. Together, both tools create an efcient, effective, and scalable solution.
Figure 4. Next Generation Tools—
Actionable Device Data

Cybersecurity Pracce #9: Network Connected Medical Devices
106Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Scanning results of ADS tools may include detailed insights into what type of device is detected, its
make, capabilities, location, application/port, and behaviors. ADS applications can solve the fundamental
inventory problem by searching, with little to no human intervention, the healthcare organization’s
network and identifying all the network devices. The solutions will also continually scan the network for
new devices that are added.
While this feature will solve the inventory problem, there are additional requirements and considerations
needed for the solution to reach cybersecurity and asset management efciency. Additional data details
need to be collected:
• How many devices are connected?
• What types of devices are they?
• Which other devices on the network are they communicating with?
• Is the device behavior normal with respect to other similar devices?
• What is the device type, manufacturer, model, modality, serial number, operating system, etc.?
Figure 4 represents the limited data obtained from medical devices when using traditional IT security
network monitoring tools. Too often discovery only yields the information on the network interface card
connecting the device to the network or non-descript information about the device.
Many devices are only intermittently connected to the network or have not yet been deployed. No
amount of automated ADS tool discovery can see these devices, yet most still possess vulnerabilities that
need to be corrected. As noted by HIPAA Security Rule, mitigations for these vulnerabilities will come in
the form of physical, administrative and technical safeguards. For example, a portable electrocadriogram
(ECG) machine not connected to the network (and contains thousands of patient records) is still at risk for
physical theft, and therefore needs controls implemented to help reduce this risk’s impact.
The combination of a CMMS tool integrated with an ADS solution allows for the cybersecurity
management of connected and non-network connected medical devices.
With ADS tools designed for medical devices, machine learning, AI and deep packet inspection can be
leveraged to provide dozens of data points that can be integrated into a CMMS and used to improve the
management of devices by device, model and eet
ADS tools can scan the network for medical devices, but they use a different approach than traditional
vulnerability scanners which can negatively impact patient safety. Instead of actively interacting with
the device, Medical Device Security (MDS) tools leverage “passive” scanning. This approach watches the
network communications between devices, servers and network equipment. This technique is sometimes
called computer learning, deep packet inspection (DPI), and AI.
DPI may capture device make, model, OS, embedded software, communication protocols, clinical
functionality, Manufacturer Disclosure Statement for Medical Device Security (MDS²) data and
connectivity. Opening and reading these proprietary packets of information is complex, but it may
provide rich contextual data on every device.
Once the basic device identication has been obtained, the device behavior is tracked and analyzed.
ADS tools can create a communications prole consisting of a variety of unprecedented data elements:
Volume, protocols, geography/location, trafc frequency, source (external or internal).
Cybersecurity Pracce #9: Network Connected Medical Devices
107Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
From these communications proles the system can establish baselines for normal behavior based on
device type. Devices that are similar are grouped for easier and more efcient management. Devices
deviating from this normal behavior will be considered anomalous and agged for inspection. Proling
and grouping devices provide for an efcient and scalable approach for managing the volume of assets and
vulnerabilities related to medical devices.
Any solution designed to mitigate and remediate the vulnerabilities of medical devices across an
enterprise will need to operate efciently and effectively. The ability to scale and apply controls at the
eet level or correlate preventative maintenance activities with security maintenance will be a direct
result of enhanced visibility into the details of each device on the network.
9.M.B: Endpoint Protections
NIST Framework Ref: PR.MA-2, DE.CM-4, PR.AC-5, PR.DS-1, PR.AC-1, PR.IP-1
As with authentication, most endpoint protection services are focused on agent-based approaches
which assume that software and patches can be installed on the devices and managed through local
or centralized servers. However, many medical devices that connect to the network lack support for
agents such as AV, antimalware, host intrusion, or even basic patching to protect them from known and
zero-day threats.
ADS solutions support a zero trust model (see 2.L.E: Micro-Segmentation/Virtualization Strategies) to
ensure access to any resource is validated and authorized. Zero trust incorporates the principle of least
privileges. The principle of least privileges is that each device or user has a specic role and function and
that access to data and services should be limited to the absolute minimum required to carry out that role
or function. Even when granted minimal access based on proper authorization, trusted devices and users
must be monitored to detect abuse of said privileges.
While restricting outbound access to remote systems and data, it is also necessary to protect individual
devices and users from incidental or deliberate access-leading to data theft, service disruption/
manipulation, ransomware, or attack proliferation. To this end, layered security is typically implemented
to restrict both inbound and outbound access to devices at various levels in the network and application
stack. If compromised, the principle of least privileges has critical relevance. A medical device such as a
blood pressure monitor should only be connected to the technologies it needs to function. For example,
the blood pressure monitor should not be connected to the HVAC system because an attacker could
leverage the HVAC system to gain access to PII or PCI data.
Where feasible, medical devices should have the following controls enabled and responsibility for these
controls may be a mix between the MDM and the HDO. For more dened responsibility information,
check out HSCC documentation Model Contract-Language for Medtech Cybersecurity (MC2):
89
• AV software: In most cases, the MDM should directly support AV software when the device uses a
commercial (non-embedded) operating system (i.e., Windows, Linux). Ensure that a compliant AV
technology is enabled. If AV cannot be implemented, compensating controls should enforce an AV
scan whenever the device is serviced prior to reconnecting to the device network.
89 Model Contract-language for Medtech Cybersecurity (MC2), Healthcare & Public Health Sector Coordinating Councils
(HSCC) (March 2022), https://healthsectorcouncil.org/model-contract-language-for-medtech-cybersecurity-mc2/.

Cybersecurity Pracce #9: Network Connected Medical Devices
108Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Local rewalls: Medical devices should be congured to communicate only with required systems, if
supported by the MDM. Unused devices and ports should be disabled if they are supported by the
manufacturer as they are only protected at the device level beneath a local rewall.
• Encryption: If supported by the manufacturer, medical devices should be encrypted at rest by default.
This will ensure the condentiality and integrity of the data in case the device is lost or stolen.
• Application allowlist: Congure medical devices, or implement software, to only allow known
processes and executables to run on the devices. This control alone can signicantly reduce the
exploitability of devices.
• Default password changes: If supported by the manufacturer, default passwords, especially those
enabling privileged access, should be changed to long, complex passwords used only for the medical
device. Do not tie unique device credentials to any general systems management credential, as
you do not want general credential compromises to affect the medical device. It is the MDM’s
responsibility to design devices not to use hardcoded or default passwords and to require a password
change on the rst use and it is the HDO’s responsibility to change passwords consistent with HDO
access management policies.
• Routine patching: The MDM and HDO share the responsibility in routine patching. The MDM’s
responsibility is to design devices to have secure, reliable update capabilities (e.g., digital signatures
for software/rmware) and to communicate when updates are available. The HDO’s responsibility is
to monitor, deploy, and track updates to devices at their facility.
9.M.C: Identity and Access Management
NIST Framework Ref: PR.AC, PR.AC-7, PR.AC-4
As much as possible, medical devices should have controls for authentication, vendor support passwords,
and remote access.
Authentication
Foundational to any IAM solution is to ensure accurate detection and tracking of each asset and user that
connects to the network for identity validation. This core requirement has mature solutions related to
managed devices and users. An explicit credential is produced to ascertain identity including certicates,
username/passwords, tokenization, and other methods that attempt to link a device/user to a trusted
entity. Many of these methods entail the use of agents or installation of software to validate identity.
However, a signicant percentage of the devices and users that connect to the network do not support
agents or explicit identity credentials. These include the ever-expanding list of IoT and other devices that
lack a user presence to submit a trusted credential at the point of entry. Even for managed devices with
an associated user, the device itself is often not authenticated (just the user of the device), which leaves a
gap in the trust of the device itself.
Common NAC systems address these gaps using MAC or IP-based authentication. The bypass of true
authentication using only the MAC or IP address is a weak attempt to uniquely track non-authenticating
devices. This leaves many organizations exposed to high risk, as there is a weak trust relationship and
exposure to spoong and inability to truly identify and audit the actual devices that are connected to
the network. ADS solutions may be able to ngerprint devices that connect to the network including
a synopsis into a device’s hardware (manufacturer, model, serial number), software (operating system,

Cybersecurity Pracce #9: Network Connected Medical Devices
109Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
version, rmware revisions), device type and function, as well as a security assessment for vulnerabilities
and risk. ADS device discovery and classication is passive and requires no agents.
Once a device is identied, these solutions continually monitor its communications for both ow data as
well as deep inspection of the communication protocols and applications to check for spoong, threat
activity, and behavioral anomalies. This ensures that even if devices can circumvent authentication,
threats are detected and can be blocked from the network.
In addition to authentication, other device context such as time, location, vulnerabilities, and posture
compliance often factor into network access decisions. ADS solutions augment the tracking of these
other elements for a comprehensive understanding of each network-connected device and to allow more
accurate access decisions based on governance and security policies.
Vendor Support Passwords
Passwords should be complex and not shared among the vendor team. A unique logon credential should
be established for each vendor employee. Ensure the manufacturer does not use the same account and
password to manage medical devices in your organization and others.
Remote Access
If remote access is required to manage medical devices, MFA capabilities should be deployed. The HDO
must accept the system access mode to be used. Depending on the deployment scenario, the device
manufacturer may be required to support remote access capabilities. Otherwise, such capabilities should
be deployed on a separate component of your existing MFA system to limit exposure if the MFA system
is compromised.
If leveraging a vendor’s remote access tool, be sure to evaluate the risk of “unattended sessions”. These
are sessions by which the vendor is permitted to access your network or medical device without any
prior authorization from the HDO. This is a useful back channel for malicious actors to leverage to
unauthorized access into enterprise information systems. If the vendor’s remote access tools are to be
activated, insist that these sessions always be “attended”. This means for any remote access connection
that will be made, there must be a HDO sponsor authorizing the access. Otherwise, the request access
will be denied.
Remote access can be broken down into basic categories: 1) extended branch/remote ofce, 2) user to
campus, and 3) user to cloud. ADS solutions do not typically monitor direct communications between
a remote user and a cloud service but do play an active role in the rst two categories. For extended
branch/remote ofce, ADS provides the same set of rich device discovery, classication, and security
analytics as devices connected to an enterprise campus network. For remote users that connect to a
campus network (and resources over a VPN or similar service), ADS provides comprehensive visibility into
all connected IPs, monitors them for risk and unexpected behaviors, and tracks access to both authorized
as well as unauthorized or high-risk targets. ADS solution’s trafc analysis allows network and security
administrators to visually monitor remote access communications by location and subnet and track
them for safe and approved behavior and quickly detect exceptions. They also monitor threat activity
in expected ows through intrusion detection services, and correlate communications to at-risk sites
through its extensive threat and reputation feeds.

Cybersecurity Pracce #9: Network Connected Medical Devices
110Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
9.M.D: Network Management
NIST Framework Ref: PR.AC-5
As much as possible, HDOs should ensure the following network management controls are enabled for
the medical devices in their networks:
• Segmentation: Given the critical nature of medical devices and your organization’s general inability
to congure them to reduce vulnerabilities, it is crucial to segment these devices separately from
general access or data center networks. The ability to restrict access to the device is essential to its
safe operation.
Dedicated, highly-restricted networks should be set up. The only trafc allowed on these networks
should be proled based on required operation of the devices connected to that network. Access to
device management systems should be heavily restricted to limit its exposure. Lastly, it is important
to ensure that these networks are segmented such that any vulnerability scanning systems are not
permitted access in a clinical setting. Given the delicate nature of medical devices, execution of a
rogue vulnerability scan could disrupt the devices.
• Micro-segmentation: This takes segmentation one step further by protecting devices from other
systems in the same network segment in addition to systems outside of their network. It is based on
defense in depth and, if supported, may be the most effective way to protect devices from network-
based attacks. Medical devices are purpose-built devices that adhere to a predened set of limited
communication patterns. They are well suited to be protected by micro-segmentation, preventing
attackers who penetrate a traditional segment from moving laterally because all unessential trafc
is restricted.
While this security strategy is effective, operationalizing micro-segmentation can be cost prohibitive.
It requires network engineers to determine the restrictions and then program those rules/policies
into the network components. With tens of thousands of devices, manually implementing and
maintaining micro-segmentation is not achievable.
ADS tools can automatically and intelligently create network policies/rules based on the monitoring of
device communication whereby devices are never trusted, and the environment is assumed to be hostile.
This approach accomplishes the most granular level of micro-segmentation: zero trust architecture
(ZTA). ZTA operates on the premise that both internal and external networks are untrustworthy with no
distinction between them. Additionally, all device access requests and communications with a device are
always veried based on the behavioral analytics obtained during the baselining process. ZTA, however
will not protect unconnected devices, or devices yet to be onboarded. ZTA is difcult to manage without
a dedicated team of IT resources. If security events or vulnerabilities are identied, these unconnected
devices must be remediated too.
Once generated, these policies can be implemented manually by staff or automatically by integration
with the target system (e.g., Cisco ISE, Firewall API, etc.). Policies can likewise be automatically created to
isolate or quarantine devices with high levels of risk or signs of compromise.
Devices with vulnerabilities, recalls, weak passwords, or signs of threats can be tagged for remediation,
and optionally protected or isolated to limit exposure. Policies/rules can be enforced based on the
connected medical device’s observed risk, known vulnerabilities, signs of IOC and their context with the
unique network itself. Mission critical devices or high-valued assets may have more stringent restrictions.

Cybersecurity Pracce #9: Network Connected Medical Devices
111Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
ADS solutions are designed to approach medical device security dynamically because the context of the
clinical network environment is always changing. Trust can change for a session or a device between
one login and the next. New devices are constantly being added and removed which introduce different
vulnerabilities to the environment. ADS solutions can identify new devices, changes in device behavior
and new IOCs.
HDOs realize several benets from micro-segmentation:
• Isolation: During cyber-attacks, network trafc is isolated, limiting access between segments.
• Monitoring: Monitoring of Internal communications, inter-segment communications, log events and
irregular device behavior.
• Compliance: Reduction of the number of systems subjected to regulation.
• Access Control: Limited access to sensitive data, prevention of privilege escalation, and
lateral movement.
As part of the segmentation strategy, review data ows and interfaces between the medical devices and
their connected systems. Be sure not to limit the essential functionality of the medical device, including
its ability to be patched remotely, if required. Device manufacturers may require installation of their own
physical networks in your organization. In these cases, access to the manufacturer’s physical network
should be limited with the same restrictions as if the HDO were implementing its own segmentation
strategy. For more dened responsibility, check out HSCC documentation Model Contract-Language for
Medtech Cybersecurity (MC2).
90
9.M.E: Vulnerability Management
NIST Framework Ref: ID.RA-1, PR.IP-12, ID.RA-5, RS.CO-5, DE.CM-8
As much as possible, medical devices should have the following vulnerability management
processes implemented:
• Vulnerability and risk categorization
• Contract negotiation
• Vulnerability disclosure programs
• Software bill of materials (SBOM) and vulnerability lookups
• Vulnerability scanning
Vulnerability and Risk Categorization
In 2016, the FDA issued the Postmarket Management of Cybersecurity in Medical Devices guidance.
91
This guidance document presents components for the proper management of medical devices after
they have been deployed in an HDO. Focusing on the risk to patient safety, this guidance stipulates
manufacturers should implement vulnerability and risk-management practices to categorize risks
according to the exploitability of the cybersecurity vulnerability and the potential to cause harm to
the patient.
90 Model Contract-language for Medtech Cybersecurity (MC2), Healthcare & Public Health Sector Coordinating Councils
(HSCC) (March 2022), https://healthsectorcouncil.org/model-contract-language-for-medtech-cybersecurity-mc2/.
91 Postmarket Management of Cybersecurity in Medical Devices, Food and Drug Administration (FDA) (October 1, 2018),
https://fda.gov/regulatory-information/search-fda-guidance-documents/postmarket-management-cybersecurity-
medical-devices.

Cybersecurity Pracce #9: Network Connected Medical Devices
112Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
HDOs should work with device manufacturers to arrive at a common understanding of the framework
for the risk categorizations. Upon disclosure of a high risk, HDOs should take escalated action to secure
the device.
Utilizing a risk-based approach to vulnerability management which permits exibility can address the
problem of scarce resources on tasks that mitigate and reduce risk to your organization.
The Common Vulnerabilities and Exposures (CVE) is a list of publicly known cybersecurity vulnerabilities
and exposures maintained by MITRE Corporation. The U.S. National Vulnerability Database is fully
synchronized with the MITRE CVE list. When a CVE is found and identied, a software company releases
a patch so users can download it and repair the vulnerability. Many HDO’s have a patch-management
solution to address patching systems in their network; however, they lack a patch validation view and
knowledge about the completeness of the patching event. CVE entries can be very helpful in identifying
vulnerable devices in the HDO environment.
With ADS tools designed for medical devices, machine learning, AI and deep packet inspection can be
leveraged to provide dozens of data points that can be integrated into a CMMS and used to improve the
management of devices by device, model and eet.
ADS tools can scan the network for medical devices, but they use a different approach than traditional
vulnerability scanners which can negatively impact patient safety.
Instead of actively interacting with the device, MDS tools leverage “passive” scanning. This approach
watches the network communications between devices, servers and network equipment. This technique
is sometimes called computer learning, deep packet inspection (DPI), and AI.
Once the basic device identication has been obtained, the device behavior is tracked and analyzed. ADS
tools can create a communications prole consisting of a variety of unprecedented data elements: volume,
protocols, geography/location, trafc frequency, and source (external or internal).
From these communications proles the system can establish baselines for normal behavior based on
device type. Devices that are similar are grouped for easier and more efcient management. Devices
deviating from this normal behavior will be considered anomalous and agged for inspection. Proling
and grouping devices provide for an efcient and scalable approach for managing the volume of assets and
vulnerabilities related to medical devices.
Any solution designed to mitigate and remediate the vulnerabilities of medical devices across an
enterprise will need to operate efciently and effectively. The ability to scale and apply controls at the
eet level or correlate preventative maintenance activities with security maintenance will be a direct
result of enhanced visibility into the details of each device on the network.
Cybersecurity Pracce #9: Network Connected Medical Devices
113Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 13. ADS Use Cases
Use Cases Monitor Analyze Secure
Undesired Trafc Watch risky ports
(e.g., 3389)
Assess appropriateness Block ports or segment
Vulnerabilities Correlate known
vulnerabilities with
existing assets (e.g., Ripple
20, Deja Blue)
Evaluate, discuss
with vendors, and
determine mitigation
Patch, block ports
or segment
Unsupported OS Identify risky devices Assess trafc—necessary
and unnecessary
Upgrade OS, replace
device or segment
Device Behavior Determine “normal
activity” baseline
Assess trafc—necessary
and unnecessary
Block unnecessary trafc
ADS tools can analyze each device in terms of potential risk to your organization, as seen in Table 13
above. This analysis can include a wide range of device traits including the identication of high-value
devices, devices with known vulnerabilities, devices that have been recalled, devices using weak or open
passwords, and weak TLS ciphers or expired certicates. For example, devices that process sensitive
information such as PHI can be identied automatically. This can be extremely efcient in supporting a
HIPAA-required risk analysis.
ADS tools can also discover signs of compromise using both known and behavioral IOC. Known indicators
can include interaction with known malicious IP addresses or domains. Alternatively, these new systems
can recognize behavioral anomalies within devices based on observed baselines in the network or
deviations from norms for a particular device proled.
Vulnerability Disclosure Programs
Each device manufacturer should have a program that informs HDOs of vulnerabilities in their devices.
These programs should have a communication channel to report information and inform parties. HDOs
should work with the manufacturers so that all parties understand the respective points of contact
between the manufacturer and the HDO.
In addition to direct communications from manufacturers, other channels exist for the disclosure of
medical device vulnerabilities. These include the CISA National Cybersecurity and Communication
Integration Center, the Health Sector Cybersecurity Coordination Center (HC3), and the Industrial
Control Systems—Computer Emergency Response Team (ICS-CERT); manufacturers can include these as
part of their vulnerability releases, as can ISACs or ISAOs with which the manufacturers participate.
92
The HDO should have a program in place to accept inbound vulnerability disclosures, evaluate the
HDO’s exposure to these vulnerabilities, and identify, alongside the manufacturers, response actions to
remediate or mitigate each vulnerability according to its level of risk.
With a well-established vulnerability disclosure program, medical device manufacturers and HDOs will
have bidirectional communication for managing medical device vulnerabilities. Communication is key
92 “Health Sector Cybersecurity Coordination Center (HC3),” HHS.gov (March 31, 2022), https://www.hhs.gov/about/
agencies/asa/ocio/hc3/products/index.html#sector-alerts.
“ICS-CERT Advisories,” CISA (Accessed June 2, 2022), https://www.cisa.gov/uscert/ics/advisories.
Cybersecurity Pracce #9: Network Connected Medical Devices
114Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
to maintaining patient safety. Table 14 provides a general rule for the response timeframes (including
interim compensating controls) for medical device vulnerabilities; this general rule is in line with
expectations in the Postmarket Management of Cybersecurity for Medical Devices guidance.
93
Table 14. Timeframes for Resolving Medical Device Vulnerabilities
Vulnerability Cricality Days
Uncontrolled Risk
• Vendor communicates to HDO; HDO
determines interim mitigation step
30 days
• Vendor produces a risk remediation solution;
HDO implements solution
60 days
Controlled Risk As dened by routine patching and
preventative maintenance
Software Bill of Materials (SBOM) and Vulnerability Lookups
Most medical devices include open-source software components and libraries. Many of these medical
devices ship with vulnerable or out-of-date software components that may never be updated, according
to the Department of Commerce’s National Telecommunications and Information Administration (NTIA).
Using SBOMs registered in your organization’s ITAM, CMMS or other systems, the HDO can compare
data from the NVD against data in your organization’s software libraries. This comparison provides the
HDO with information on current potential vulnerability postures in the medical device space.
A simple search of the NVD can be conducted by using the web interface located on NIST’s website.
94
This search tool allows HDOs to look up vulnerabilities in products that they currently have. It does not
require SBOM material to be preregistered.
To support the development of an automated solution, in July 2018, the U.S. National Telecommunications
and Information Administration (NTIA) launched a multi-stakeholder initiative to improve software
component transparency across myriad industries, including medical device technology.
95
Their goal is
to standardize the process for sharing the data on the components within devices. There is little visibility
into the supply chain which is problematic for security. President Biden’s Executive Order on Improving
the Nations Cybersecurity signed in May of 2021 specically promotes the continued development of the
NTIA SBOM initiative.
96
A proof of concept is being tested to address this issue. Prestigious academic medical centers using ADS
solutions and CMMS tools have worked with renowned medical device manufacturers under the direction
of the NTIA in a public/private partnership to automate the creation and ingestion of a SBOM. MDM’s
now can produce SBOMs containing medical device component detail, which can then be automatically
93 Postmarket Management of Cybersecurity in Medical Devices, Food and Drug Administration (FDA) (October 1, 2018),
https://fda.gov/regulatory-information/search-fda-guidance-documents/postmarket-management-cybersecurity-
medical-devices.
94 “National Vulnerability Database,” NIST (Accessed June 2, 2022), https://nvd.nist.gov/.
95 “NTIA Software Component Transparency,” National Telecommunications and Information Administration (NTIA)
(April 28, 2021), https://www.ntia.doc.gov/SoftwareTransparency.
96 Executive Order No. 14028, (May 12, 2012), https://www.whitehouse.gov/brieng-room/presidential-
actions/2021/05/12/executive-order-on-improving-the-nations-cybersecurity/.
Cybersecurity Pracce #9: Network Connected Medical Devices
115Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
parsed and ingested from a vulnerability source into the ADS or CMMS technology solutions which
provide indexes to devices within the HDO’s clinical network. Advancements like this will have an
unprecedented impact on reducing the risk of vulnerabilities like Ripple 20 (which identies the Vxworks
operating system within 2 billion devices, many of which are medical devices).
Vulnerability Scanning
WARNING: UNLESS APPROVED BY THE DEVICE VENDORS, THIS ACTION SHOULD BE TAKEN
WITH EXTREME CAUTION DUE TO THE POTENTIAL IMPACTS ON MEDICAL DEVICES WITHIN THE
PRODUCTION ENVIRONMENT. HDOS SHOULD NOT ATTEMPT TO CONDUCT VULNERABILITY
SCANS UNLESS ABSOLUTELY CERTAIN THAT THE MEDICAL DEVICE IS NOT IN PRODUCTION, IS
NOT CURRENTLY IMPLEMENTED IN A CLINICAL SETTING, AND IS NOT CONNECTED TO PATIENT.
The nal action an HDO can take to understand its vulnerability posture is to conduct vulnerability scans
against the medical devices.
The primary opportunities to conduct vulnerability scans against medical devices are:
• When the device is rst procured and tested before deployment in the production environment
• When a device is taken ofine for preventative maintenance and routine patching
• During the utilization of an ADS tool
In all scenarios, it is important for the device to be in a highly controlled setting and not connected to a
patient. A vulnerability scan can be congured to prole the device and determine whether potential
vulnerabilities exist, or to conrm that vulnerabilities have been mitigated as part of a remediation or
patching plan.
To conduct such an exercise, it is best for the cybersecurity team to work with the clinical engineering
teams and establish a proled scan template in the vulnerability management software. This template
should allow the scan to be executed only against a specic nonproduction network and only by specic
individuals. To provide further assurance that the vulnerability scan cannot cause harm to the medical
device while it is connected, the scanners’ IP addresses should be blocked as part of the segmentation
strategy noted above.
When these preparations are complete, the clinical engineering teams can be granted access to the
scanning software in a restricted manner that allows the scan to be run only against the network used
for preventative maintenance. Vulnerabilities discovered can be shared with the cybersecurity ofce
to determine the relative risks. Upon classication of these risks, the teams should contact the device
manufacturer and work together to develop and implement a remediation plan.
9.M.F: Contacting the FDA
NIST Framework Ref: RS.AN-5
If an HDO discovers (or is notied) of a high-risk cybersecurity
vulnerability and cannot receive support from the medical device
manufacturer to mitigate this risk, the HDO has recourse to contact
the FDA directly to le a complaint concern about the vulnerability.
FDA contact should be limited to critical or high-risk scenarios,
especially those with the potential to cause harm to patients.
The Center for Devices and
Radiological Health emergency
contact information is
provided below:
Email: [email protected]
Phone: (301) 796-8240 (24 hours
x 7 days per week)
Cybersecurity Pracce #9: Network Connected Medical Devices
116Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Large Organizations
9.L.A: Security Operations and Incident Response
NIST Framework Ref: PR.IP-9, DE.CM-8, DE.CM-1, DE.CM-7
Expanding on the SOC and IR processes found in Cybersecurity Practice #8: Security Operations Center
and Incident Response, HDOs can provide additional monitoring, detection, and response activities
around their medical device ecosystems. HDOs should monitor for malicious activity into and within
the segment using the segmentation strategy outlined previously. To provide visibility into the daily
operations of the medical device systems, the following sources should be congured to send activity and
access logs to the HDO’s log management systems, SIEMs, or both:
• Firewalls providing segmentation to the medical device network segment
• Information systems that control the operation of the medical devices
• The full context of possibly impacted devices, including devices only intermittently connected or yet
to be onboarded (as these devices are still susceptible to vulnerability if left uncorrected)
• Netow data from the medical device network segment
• Intrusion prevention systems in front of the medical device network segment
• Logs from any deception technology deployed in the medical device network segment
Security Orchestration and Automated Response (SOAR)
HDOs should strive to consolidate all device information into one cloud-based CMMS. By replacing
multiple maintenance management systems and databases containing disparate data elements into on
CMMS, an HDO can position itself for a single device inventory that is integrated with ADS solutions to
orchestrate the remediation of cybersecurity events. This includes preventative maintenance, corrective
maintenance, contract, cost of ownership, capital planning, asset discovery, security data, and events.
This CMMS of consolidated data are used to correlate events and vulnerabilities against device
records from the NIST Cybersecurity Framework 1.1, NVD, CPE, and Mitre CWE.
97
For additional
preparedness information refer to the Medical Device Cybersecurity Regional Incident Preparedness and
Response Playbook.
98
Security events can be provided in a shared view to healthcare technology management (HTM) and IT
teams, showing the device(s) affected, the device owner and the device location, and the latest software
and rmware versions. Rules-based identication algorithms can correlate all affected devices by the
event or vulnerability and information like whether the device generates PHI data or stores PHI data.
Just as the clinical engineering team responds to preventative maintenance work orders in the CMMS
system, HTM and network engineers can respond to a CMMS’ security maintenance work orders.
97 Cybersecurity Framework Version 1.1, NIST (April 2018), https://www.nist.gov/cyberframework/framework.
“National Vulnerability Database,” NIST (Accessed June 2, 2022), https://nvd.nist.gov/.
“Common Platform Enumerations (CPE),” NIST National Vulnerability Database (NVD) (Accessed June 2, 2022),
https://nvd.nist.gov/products/cpe/search.
“Common Weakness Enumeration (CWE),” MITRE (Accessed June 2, 2022), https://cwe.mitre.org/.
98 “Medical Device Cybersecurity Regional Incident Preparedness and Response Playbook,” MITRE (October 2018),
https://www.mitre.org/publications/technical-papers/medical-device-cybersecurity-regional-incident-preparedness-
and.
Cybersecurity Pracce #9: Network Connected Medical Devices
117Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Coordinated remediation processes (via workow management) provides security context and event
impact, including what patch, conguration change, or mitigating controls are required to then determine
the remediation priority.
Baselining Devices
Practice 8.L.D: Baseline Network Trafc specied the need for understanding device communications.
Monitoring the communications of medical devices is imperative to establishing their security. Once an
HDO has identied all connected medical device assets, determining its purpose in the enterprise and
understanding its normal behavior patterns is the next step in effective asset management. Mapping
communications patterns and baselining device behavior is crucial to identifying anomalous behaviors.
The behavior of each device must be understood to ascertain the degree of exposure to internal and
external threats. These pieces of data are extremely difcult to obtain without automated tools..
Network Behavior
• Does the device communicate with the manufacturer for updates and patches?
• With what other devices is it communicating?
• Is the device type isolated to communication within the VLAN?
• Are communications normal for this device type?
Understanding the clinical context with respect to medical device cybersecurity is imperative. Beyond
security, devices containing ePHI are required to be identied as a part of a HIPAA Risk Assessment.
Consider the following:
Clinical Context
• Does the device transfer or store PHI?
• What is the consequence of failure—inappropriate therapy or misdiagnosis?
• What is the equipment class? Diagnostic?
• Which connections are clinical and non-clinical?
Security efforts must avoid interfering with critical clinical dataows. However, once organizations can
recognize these clinical workows, the cybersecurity or HTM will be able to identify anomalies that could
negatively impact patient care (resulting in direct patient harm).
Proling and Grouping Devices
Managing devices at a group level is necessary to effectively manage tens of thousands of medical device
requirements. Healthcare organizations need to collect a wide range of data on every connected device
to group and compare devices on the network. This includes decoding dozens of device and industry-
specic protocols to analyze detailed application-level behavior. Traditional security tools are limited to
traditional protocols. Determining normal communications is challenging.
Determining normal communications within a device type by comparing communication ows is near
impossible with traditional security tools. As an example, XYZ Health Systems has 100 Infusion Pumps,
99 of which are talking to the manufacturer in India and 1 is communicating with someone in Kiev.
ADS solutions are helping healthcare organizations reduce their attack surface by providing a clear
understanding of what is on the network and controlling unnecessary communications and services. By
passively monitoring device communications, organizations can associate attributes to the device: ports,

Cybersecurity Pracce #9: Network Connected Medical Devices
118Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
services, and protocols. These new attributes, or data elements, can be used to index and better manage
the hardware assets in the asset inventory.
Organizations can automatically baseline the behavior of devices in the network as well as known
behavior of similar devices. ADS solutions can baseline what other assets with which a device needs
to communicate to accomplish its function. It can understand which protocols are used, verifying the
communications are safe and not part of threat activity. Cybersecurity or HTM can create detailed
policies/rules that will limit a device’s communication to only those required to perform its given function.
See the Segmentation section of 9.M.D: Network Management for more detail on creating policies
and rules.
Mapping the device communication ow allows ADS solutions to provide actionable insights across
millions of devices within healthcare’s hyper-connected enterprise. To accomplish this, it requires
comprehensive real-time collection, correlation, and analysis of vast amounts of information about
each device.
Deep Packet Inspection
Data packets transmitted throughout networks contain far more contextual than merely the sender
and recipient devices. Captured network trafc is analyzed by ADS tools to retrieve rich data from
devices, including:
• Device classication/grouping: manufacturer, device type, model, modality, and serial number
• Operating system information: software version, patches, components, and antivirus software
• Network information: VLAN/subnet, wireless access points, connectivity, switch ports, and
comparisons between peer devices
Analysis of device communication data from deep packet inspection can reveal the transmission “ows” to
and from each device monitored by the ADS. Such granularity allows IT and HTM personnel to visualize
device interactions from varying levels or perspectives, such as:
• Device level ow: location, connection attempts, last connection, usage, sessions, and data rate
• Communications ow: baseline behavior, group comparisons, and anomalies
• Internal communications: malware signatures
• External communications: real-time comparison of device patterns, and communication with
hostile sites
ADS solutions are designed to collect and analyze device and system data from multiple sources within
the enterprise, including:
• Network infrastructure data from switches, routers, WLAN controllers, NAC solutions, etc.
• On-demand vulnerability scans for onboarding as well as information collected from other periodic
vulnerability scan reports
• Device probes like Simple Network Mapping Protocol (SNMP) for inherent device information from
various MIB repositories
• Protocol decodes of proprietary protocols like DICOM, Modbus, and patient monitoring systems
• User and location information (including Active Directory users with roles and privileges, and location
feeds, etc.)
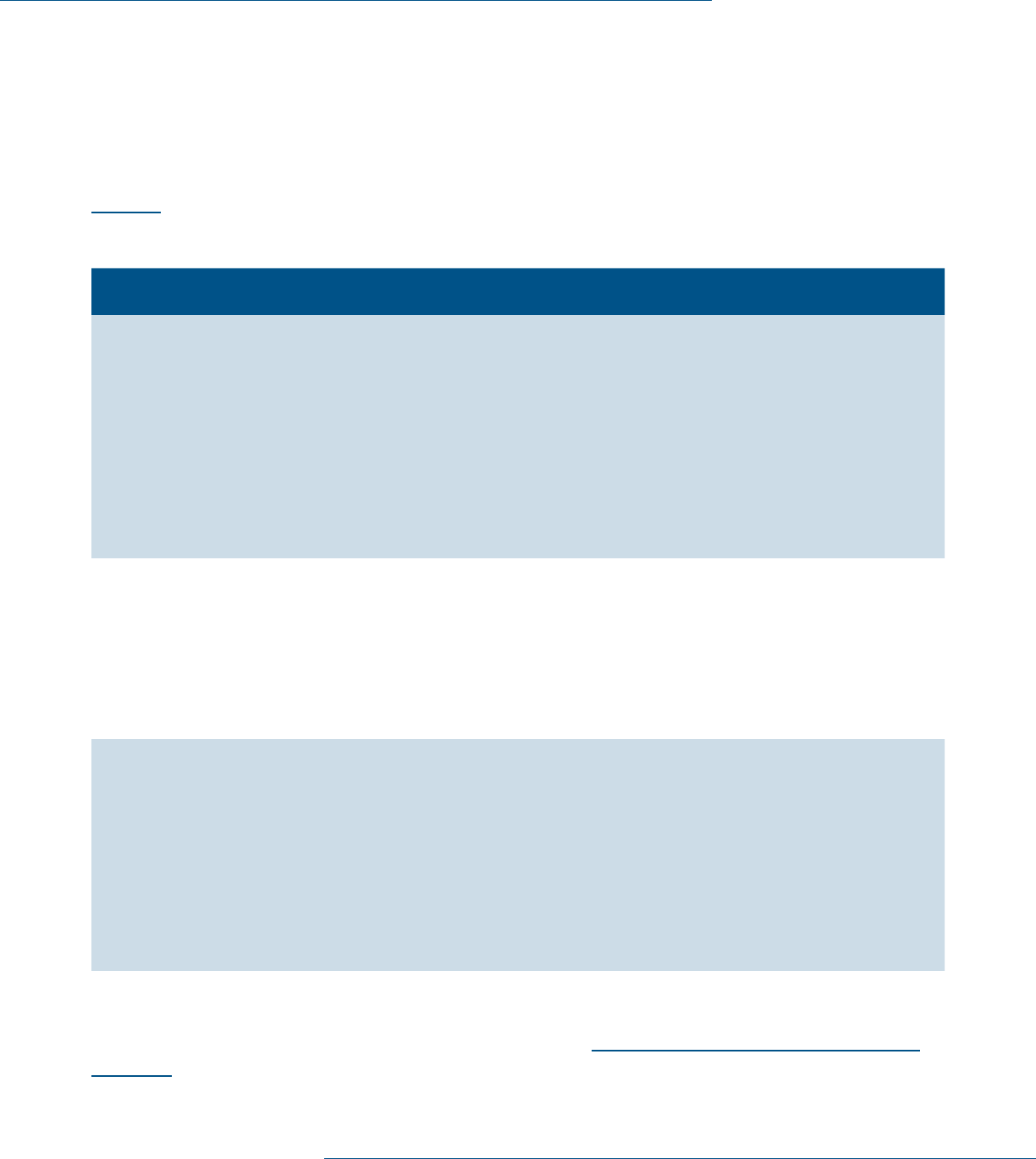
Cybersecurity Pracce #9: Network Connected Medical Devices
119Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
• Full packet capture data from backbone core routers ) including all le transfers, HTTP sessions, peer-
to-peer trafc, client-server trafc, and application-level interactions)
• Network layer control plane protocols (e.g., Dynamic Host Conguration Protocol [DHCP])
• Utilization and performance data like frequency and duration of operation and connection attempts
• Parsing results from well-known data plane signatures from security vendors
Using these logs as a source, plays can be enumerated and added into IR playbooks, as described below in
Table 15.
Table 15. Incident Response Plays for Attacks Against Medical Devices
Play Category Play Descripon Source Data
Reconnaissance Vulnerability
scanning
sweep of
medical device
segment
Scan large numbers of
vulnerabilities across the
medical device network.
May involve scanning a
single server over multiple
ports or scanning multiple
servers over a single port.
• Medical device
management system
• IDS/IPS logs in front of the medical
device network, congured to
detect vulnerability scanning
• Firewall logs in front of the medical
device network
• Netow data from within the
medical device network
Lateral
Movement
Detection
of unknown
source clients
accessing
medical
device remote
access ports
Detect attacks coming
from sources outside
of known management
sources attempting to gain
access to remote access
ports (e.g., FTP, SSH).
• Firewall logs in front of the medical
device network
• Network data from within medical
device network
Lateral
Movement
Triggered
decoy within
medical device
network
Respond to decoy triggers
being communicated
from within or across
the medical device
network segment.
These communications
should not occur; they
indicate malicious or
broken processes.
• Deception technology logs from
within the medical device network
• Firewall logs in front of the medical
device network
• Network data from within the
medical device network
If an HDO experiences a security incident and requires the assistance of the manufacturer, the
HDO should leverage their contact information. This should have been established as part of the
vulnerability disclosure program, outlined within sub-practice 9.L.A: Security Operations and Incident
Response above.

Cybersecurity Pracce #9: Network Connected Medical Devices
120Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
9.L.B: Procurement and Security Evaluations
NIST Framework Ref: ID.SC
HDOs should establish a set of cybersecurity requirements during the acquisition of medical devices.
These requirements should be memorialized in your organization’s contracting processes and
implemented through the supply chain and procurement functions. Cybersecurity requirements should
be incorporated into prospective procurements through vendor requests for information (RFIs) or
requests for proposals (RFPs). These requirements should include high-value items such as supported
and patchable operating systems, AV or allowlisting, no hardcoded or default passwords, and minimal use
of administrative privileges.
Organizations should set policies and procedures that require procurements of technology and
integrations (including medical devices) to undergo security evaluations as part of the HDO’s supply
chain process. Implementing cybersecurity evaluation as part of the supply chain process provides an
opportunity for your organization to understand, evaluate, and mitigate cyber risks prior to technology
deployment. When a security evaluation is undertaken, the scope of the assessment should include all the
other devices required for the device to perform its clinical functions. As an example, an assessment of
an infusion pump system would evaluate both the infusion pump and the server to which it connects for
the formulary update. Another example would an instance where the assessment of an MRI device would
place the specialized workstations that control its operation in scope.
Security Evaluation
An initial phase of the medical device acquisition process should be a security evaluation of the device.
This evaluation should uncover any risks or aws in the current design of the medical device and establish
transparent communications between stakeholders from the supply chain, clinical engineering, and
manufacturing functions. The HDO should insist on receiving a MDS
2
.
99
The MDS
2
is an industry standard
format developed by the Health Information Management and Systems Society and the American College
of Clinical Engineering that has been adopted by most manufacturers. It provides a list of comprehensive
cybersecurity questions for medical devices, with responses from the manufacturer of the device in
question. Questions in the MDS
2
include the following:
• Can this device display, transmit, or maintain private data (including electronic PHI/PII)?
• Can the medical device create an audit trail?
• Can users be assigned different privileged levels within an application based on ‘roles’ (e.g., guests,
regular users, power users, administrators)?
• Can the device owner/operator recongure product security capabilities?
A copy of the latest MDS
2
can be found on the Association of Electrical Equipment and Medical Imaging
Manufacturers’ website.
100
Answers to these questions assist the HDO in completing a meaningful
evaluation of the medical device. The HDO should also consider requesting an SBOM and an Enterprise
Architecture Diagram to create a complete Vendor Assessment Package.
99 Manufacturer Disclosure Statement for Medical Device Security, NEMA (October 28, 2019), https://www.nema.org/
Standards/view/Manufacturer-Disclosure-Statement-for-Medical-Device-Security.
100 The Association of Electrical Equipment and Medical Imaging Manufacturers (MDS
2
) form HN 1-203, rev.2019, NEMA
(2019), https://www.nema.org/Standards/ComplimentaryDocuments/MDS2-Worksheet.xlsx.
Cybersecurity Pracce #9: Network Connected Medical Devices
121Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
The HTM collaborates with the security team to triage each device during the intake process. It is often
benecial to break the type of request into four categories:
• New Device—Unknown Risk
• Repeat Purchase—Unknown Risk
• Repeat Purchase—Known Risk
• No Security Assessment Required
This will allow the HDO to identify mitigating controls determined to stop new risk being entered into the
environment. By focusing the HDO’s limited resources on devices with “unknown risk”, this process will
focus efforts to reduce the new entering the system risk during the onboarding process. The product of
the risk assessment process should be a prole of remediation plans to reduce each risk associated with
that specic device.
Risk Scoring
Current methods for analyzing identied cyber vulnerabilities tend to apply to traditional IT and focus
on the impact to a system’s condentiality, integrity, and availability (CIA) to discern end-user risks. The
CVSS score is designed to provide an overall measurement that can be used for making HTM decisions
helping to prioritize mitigation efforts in a consistent and measurable manner. Although sufcient for
evaluating traditional IT systems, this scoring system fails to consider the operational ramications for
complex systems-of-systems like those found in a clinical environment.
The risk scoring system does not adequately consider the context of the environment for identied
vulnerabilities. Consequently, organizations may improperly prioritize mitigation efforts. For example,
while the CVSS evaluates the severity of an identied vulnerability in the context of system impact, for
medical devices, it does not take into consideration the impact to patient safety—the true indicator of the
severity of the vulnerability.
ADS solutions should be considered since they provide a multi-factorial risk score for every device on
the network. These factors include the probability of a compromise, criticality, CVE, device properties,
connectivity, etc. These factors are combined into a comprehensive, clinical network aware, context
sensitive vulnerability management platform based on the needs of each device.
Contract Negotiation
Contracts are an essential component of good risk reduction when it comes to medical devices. It is
benecial for the HDO’s cybersecurity team to review and provide input towards the contract with the
manufacturer. This should occur in tandem with the supply chain and legal. Negotiations should highlight
key security requirements from the HDO. These requirements should reference the FDA’s Postmarket
Management of Cybersecurity for Medical Devices guidance and industry standards describing components
that are critical for the safe operation of the devices.
101
Armed with the results of the cybersecurity
evaluation, scenarios to resolve any unmitigated risks should be included in the contracting process to
limit the HDO’s liability, especially with constraints around the HDO’s ability to alter the medical devices.
The Health Sector Coordinating Councils’ Joint Security Workgroup released a publication titled Model
101 Postmarket Management of Cybersecurity in Medical Devices, Food and Drug Administration (FDA) (October 1, 2018),
https://fda.gov/regulatory-information/search-fda-guidance-documents/postmarket-management-cybersecurity-
medical-devices.

Cybersecurity Pracce #9: Network Connected Medical Devices
122Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Contract-language for Medtech Cybersecurity (MC2).
102
In this publication, HDOs and MDMs provide agreed
upon contract language and a maturity model. This is designed to assist purchase contract negotiations
providing a clearer reference for obligations, accountability, and liability.
Additionally, procurement should be notied of device performance and risks discovered after the
contracting process when a device is in use. Mechanisms for communication of these vulnerabilities
found in existing devices should be conveyed back to procurement to include in the front-end security
evaluation and standard contract language.
SBOM
The HDO should request an SBOM as part of the procurement process. The SBOM is a list of software
components that the medical device comprises. It can be thought of as a list of software libraries that
make up the device, like the ingredients of a recipe. Understanding the software libraries that make up
the device allows the HDO to comprehend the impact of vulnerabilities announced by the NVD.
End of life (EOL)/End of support (EOS)
Over time, the effectiveness of medical devices will diminish, especially as hardware and software ages
and is eventually decommissioned. As part of the evaluation of these devices, manufacturers should
disclose to the HDO their life expectancy, which forms part of the HDO’s cybersecurity management
plan. The plan should include an expectation for when the EOL and EOS of the devices will occur. If there
are no EOLs or EOSs established, as best practice, the manufacturers should try to provide the HDO
at least three years in advance of EOL or EOS. HDOs are responsible for making risk-based decisions
about devices nearing EOL or EOS. In most cases, when a device becomes unsupported, or legacy, the
device should be replaced as part of established asset refresh cycles. In some cases, it is not possible to
replace legacy devices due to nancial or other resource constraints. If this is the case, the HDO should
implement compensating controls- with the understanding that the devices will no longer be supported by
the manufacturer, and their decommissioning should be strategically planned.
In 2019, the Health Sector Coordinating Council released a new publication, the Health Industry
Cybersecurity Supply Chain Risk Management Guide (HIC-SCRiM).
103
This publication describes
processes and techniques for managing all third-party risk. The techniques provided will also assist HDOs
in medical device procurement.
Key Mitigated Threats
1. Attacks against network connected medical devices
102 Model Contract-language for Medtech Cybersecurity (MC2), Healthcare & Public Health Sector Coordinating Councils
(HSCC) (March 2022), https://healthsectorcouncil.org/model-contract-language-for-medtech-cybersecurity-mc2/.
103 Health Industry Cybersecurity Supply Chain Risk Management Guide (HIC-SCRiM), Healthcare & Public Health Sector
Coordinating Councils (HSCC) (September 2020), https://healthsectorcouncil.org/hic-scrim-v2/.
Cybersecurity Pracce #9: Network Connected Medical Devices
123Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Suggested Metrics
• Number of medical devices not currently segmented on wireless or wired networks, measured monthly.
The goal is to limit medical devices on the general access network, data center network, or other
locations that do not meet the requirements of specic network segmentation strategies.
• Number of unmitigated high-risk vulnerabilities on network connected medical devices, measured
monthly. The goal is to reduce the number of unmitigated risks to as near zero as possible. Each high-
risk vulnerability should have a remediation action plan, as dened in Cybersecurity Practice #7:
Vulnerability Management.
• Number of medical devices procured that did not receive security evaluation, measured monthly. The
goal is to reduce the number of procurement actions without security evaluation to as near zero as
possible. Share this metric with your supply chain and clinical engineering departments to ensure the
procure process is executing as intended.
• Number of medical devices that do not conform to basic endpoint protection cybersecurity practices,
measured weekly. The goal is to reduce the number of medical devices that do not meet basic hygiene
management practices or to implement practices for these devices. It is not always possible to
reduce this number to zero. Mitigating factors should be employed to keep it as low as possible.
• Number of devices that have unknown risks due to lack of manufacturer-disclosed information, measured
monthly. The goal is to ensure that device manufacturers have vulnerability disclosure programs and
that your organization is privy to them.

124Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Areas of Impact
N/A
Medium Sub-Practices
10.M.A Policies
10.M.B Cybersecurity Risk
Assessment and
Management
10.M.C Security Awareness and
Training
Large Sub-Practices
10.L.A Cyber Insurance
Key Threats Addressed
• Social engineering
• Ransomware attacks
• Loss or theft of equipment
or data
• Insider, accidental or
malicious data loss
• Attacks against network
connected medical
devices that may affect
patient safety
405(d) Resources
• Prescription Poster:
Cybersecurity Policies
Cybersecurity Pracce #10:
Cybersecurity Oversight
and Governance
Cybersecurity policies must be established for the workforce
to understand how they are expected to behave with regard to
cybersecurity. These policies should be written for the various
user audiences that exist in your organization. It is important to
recognize the differences between the general workforce user, IT
user, and high-prole or high-risk users (e.g., nance, HR, or health
information management).
To set proper expectations, organizational policies should support
new cybersecurity hygiene controls. Without such policies, it may
be unclear to the workforce what level of adherence is required and
what activities put your organization at risk for the threat types
discussed in this document.
Several policy templates have been provided in the HICP package’s
Resources and Templates document.
Sub-Practices for Medium-
Sized Organizations
10.M.A: Policies
NIST Framework Ref: ID.GV-1
All organizations should maintain a baseline of core cybersecurity policies. These policies will dene the
expected behaviors of employees within your organization as it relates to cybersecurity practices. The
policies should be reviewed periodically (and at regular intervals), dened by your organizational policy
governance processes. A sample set of core policies is noted below in Table 16.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
125Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Table 16. Example Cybersecurity Policies for Consideration
Policy Name Descripon User Base
Roles and
Responsibilities
Dene all cybersecurity roles and responsibilities throughout
your organization. This includes who will establish policy and
who will implement and conduct security practices.
• All users
Education and
Awareness
Dene the mechanisms that will be used to train the workforce
on cybersecurity practices, threats, and mitigations. Ensure
education includes common cyber-attacks (such as phishing),
lost/stolen devices, and methods for reporting suspicious
behavior on individual computers.
• All users
• Cybersecurity
department
Acceptable Use/
Email Use
Describe actions that users are permitted and not permitted to
take. Explicitly dene how email is to be used.
• All users
Data Classication Dene how data are to be classied, with usage parameters
around those classications.
• All users
Personal Devices Dene your organization’s position on the use of personal
devices (i.e., BYOD). If these are permitted, establish
expectations for how the devices will be managed.
• All users
Laptop, Portable
Devices, and
Remote Use
Dene policies for the security of mobile devices and how they
are to be used in a remote setting.
• All users
• IT department
Incident Reporting
and Checklist
Dene user requirements to report suspicious activities
within your organization. Dene the responsibilities of the
cybersecurity department for managing incidents.
• All users
• Cybersecurity
department
Disaster Recovery
Plan (DRP)
Dene the standard practices for recovering IT assets in the
case of a disaster, including backup plans.
• IT department
IT Controls
Policies
Describe the requirements for IT security controls in a series of
policies or a single long policy. Examples include access control,
identity management, conguration management, vulnerability
management, and data center management.
• IT department
IT Acquisition
Policy
Dene the actions that must be taken to ensure proper
identication and protection of all IT assets purchased by
your organization.
• Supply chain/
procurement
users
• IT department
Social Media Dene what information about employee job they can
include on accounts such as LinkedIn and others. Include
recommendations for personal security settings.
• All users

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
126Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
10.M.B: Cybersecurity Risk Assessment and Management
NIST Framework Ref: ID.GV-1
A cybersecurity risk assessment helps your organization measure the likelihood of known threats and
vulnerabilities compromising data and information assets. The risk assessment is a tool an organization
can leverage to prioritize mitigation, addressing gaps in cybersecurity safeguards. This is used to put
controls in place, reducing the risk to an acceptable level. A risk assessment is an important step in
protecting your workers and organization, as well as complying with the law. A risk assessment helps you
focus on the risks that really matter and prepare for what could go wrong. A risk assessment can help
your organization understand potential risks, identify, and prioritize the risks that need to be addressed.
This should not be done in a silo, rather as an organizational collaborative effort.
Managing the security risks associated with the healthcare industry’s growing reliance on IT is a
continuous challenge. HIPAA Security Rule, Centers for Medicare and Medicaid (CMS) Promoting
Interoperability Program (formerly known as ‘Meaningful Use’), and several states’ data protection
requirements for PII require healthcare organizations to conduct a formal risk analysis.
There are several frameworks available when conducting a risk assessment. The Ofce for Civil Rights
(OCR) identies risk analysis as the foundational element in the process of achieving compliance, and it
establishes several objectives that any methodology adopted must achieve. There are numerous methods
of performing risk analysis and there is no single method or “best practice” that guarantees compliance
with the HIPAA Security Rule.
104
Some examples of steps that might be applied in a risk analysis process
are outlined in the NIST 800-30 Guide for Conducting Risk Assessments and the NIST Cybersecurity
Framework.
105
Key to the effectiveness of the risk assessment is to identify all IT assets across your
organization that handles PHI; and, to ensure the scope of the risk assessment captures the threats or
vulnerabilities that could jeopardize the condentiality, integrity, and availability of PHI. To do this, be
sure to document:
• the threats and vulnerabilities to the information system;
• the potential impact and the effectiveness of existing safeguards and controls; and
• the likelihood that the threat or vulnerability could compromise data or information system assets.
It’s important to remember that performing a risk assessment is an ongoing process and one in which
an organization:
• regularly reviews its records to track access to PHI and detect security incidents;
• periodically evaluates the effectiveness of security measures that are in place; and
• regularly evaluates potential threats and vulnerabilities to PHI.
Healthcare organizations have struggled to nd effective ways to ensure cybersecurity threats affecting
their operations (driven by human action, mother nature, or technology aw), are fully implemented
104 “Security Rule Guidance Material: Guidance on Risk Analysis,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/
security/guidance/guidance-risk-analysis/index.html.
105 SP 800-30 Rev. 1; Guide for Conducting Risk Assessments, NIST (September 2012), https://csrc.nist.gov/publications/
detail/sp/800-30/rev-1/nal.
“Cybersecurity Framework,” NIST (Accessed June 1, 2022), https://www.nist.gov/cyberframework.
Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
127Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
with appropriate controls to mitigate the risks. Enterprise Risk Management (ERM) can help identify,
communicate, and categorize an organization’s top risk areas.
106
What do cybersecurity and privacy leaders need to know
about the requirement for a risk assessment?
1. An RA should be the rst requirement in any security program or framework. It informs and
measures how well controls are working to mitigate risk and reduce liability. Not having an effective
RA is like not having a foundation to your home. Without a risk assessment, you are making decisions
based on an incomplete picture. In addition, both HIPAA Security Rule, and in some cases, state law
requires cybersecurity management. The risk assessment is a good starting point to meeting your
regulatory requirements.
2. An organization’s leadership team plays a central role in ensuring resources are properly allocated to
the most vulnerable areas of your organization. Proactive risk management will preserve and protect
your organization’s nancial viability and human assets. Risk management processes should be put in
place to protect your organization’s limited budget and resources.
3. Understanding risk, policy imperatives, and architecture are the three pillars that any successful
cybersecurity program should be built upon. Without each leg, the stool becomes unbalanced
and falls.
4. Risk assessment informs and measures how well controls are working when mitigating risk
and reducing lability. When performed correctly, it is the most useful tool for managing and
reducing costs.
5. The risk assessment is almost always the rst document requested by an investigator in an audit,
compliance review or investigation of a breach. It answers two questions: did you know the risk in
advance of the investigation; and did you plan to do anything about it?
6. Risk assessment is most benecial when objectively conducted with due diligence.
7. Have a multi-disciplinary team to identify risks in an organization. A cross section of leaders will add
value and identify something that others may not be aware of.
8. Calculate a risk rating for each threat to create a grading of risk (high, medium, low) relative to the
overall impact and likelihood should the threat be activated.
9. A risk assessment is a tool for building trust in other third-party relationships and business
partnerships. Being able to demonstrate your organization has completed a risk assessment is part of
building trusted partnerships.
10. A risk assessment will foster effective customer communications regarding quality and safety issues,
thereby reducing potential nancial losses associated with claims.
Conducting a risk assessment correctly and periodically is critical to having and building an informed
security program. Done well, it can reap many benets from saving dollars, to avoiding compliance
issues, and mitigating potential causes of disruption. Simply put, it helps protect your business and
your investment.
106 Enterprise Risk Management is an effective organization-wide approach to addressing the full spectrum of your
organization’s signicant risks by understanding the combined impact of risks as an interrelated portfolio rather than
addressing risks only within silos.” See “Circular No. A-11.” Executive Ofce of the President Ofce of Management
and Budget (OMB). Section 260. August 2022. https://www.whitehouse.gov/wp-content/uploads/2018/06/a11.pdf.
Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
128Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
For more information on risk assessments, review the Security Risk Assessment (SRA) Tool from
HHS ONC.
107
Additionally, NISTIR 8286: Integrating Cybersecurity and Enterprise Risk Management (ERM) published
in October 2020 is a comprehensive reference.
108
10.M.C: Security Awareness and Training
NIST Framework Ref: ID.GV-1
Organizations determine the appropriate content of security awareness training and security
awareness techniques based on the specic organizational requirements and the information systems
to which personnel have authorized access. The content includes a basic understanding of the need for
cybersecurity and user actions to maintain security and to respond to suspected security incidents. The
content also addresses awareness of the need for operations security. Security awareness techniques
can include displaying posters, offering supplies inscribed with security reminders, generating email
advisories/notices from senior organizational ofcials, displaying logon screen messages, and conducting
cybersecurity awareness events.
109
Also consider creating a cyber champion program within your
organization. This is a great way to increase engagement across your organization.
One method for establishing a Security Awareness Program is to designate key stakeholders within
your organization as Cybersecurity Change Leaders, or Cybersecurity Ambassadors. It’s recommended
to select stakeholders who are engrained in the culture of your organization and have a passion for
cybersecurity. Program elements might include the following:
• An onboarding and training program, with outlined roles and responsibilities of the stakeholder
• Development of cybersecurity awareness materials for delivery and distribution by the Cybersecurity
Change Leader
• Regular touch points with Cybersecurity Change Leaders (either in a group setting or individually), to
promote communication and maintain relationships
• Encouragement of feedback from the Cybersecurity Change Leader to the awareness team.
Adjustment of outreach based on these recommendations, with special attention dedicated to
understanding the best channels of cybersecurity awareness content
Please also refer to Cybersecurity Practice #1: Email Protection Systems, 1.M.D: Workforce Education,
for additional information on awareness and training programs.
107 “Security Risk Assessment Tool,” Ofce of the National Coordinator for Health Information Technology (ONC)
(February 15, 2022), https://www.healthit.gov/topic/privacy-security-and-hipaa/security-risk-assessment-tool.
108 Kevin Stine, Stephen Quinn, and Robert Gardner, NISTIR 8286: Integrating Cybersecurity and Enterprise Risk Management
(ERM), NIST (October 2020), https://csrc.nist.gov/publications/detail/nistir/8286/nal.
109 “NIST Risk Management Framework: SP 800-53 Controls and SP 800-53B Control Baselines Resources for
Implementers,” NIST (Updated May 26, 2022), https://csrc.nist.gov/Projects/risk-management/sp800-53-controls.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
129Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Sub-Practices for Large-Sized Organizations
10.L.A: Cyber Insurance
NIST Framework Ref: ID.GV-1
Cyber insurance is no longer about risk transference through the purchase of a policy that an organization
will hopefully never use. Due to the increase in ransomware attack impacts, cyber insurance providers
have undertaken a signicantly more proactive approach to both protect their businesses and the
organizations they underwrite. The relationship has changed from a transactional activity to an
ongoing relationship.
This approach aligns with the ongoing lifecycle of improving and maturing cybersecurity programs.
Before the numerous ransomware attack payouts, insurance company questionnaires asked basic
questions about system security, PCI-DSS compliance, and whether there were any reportable data
breaches. They did not ask detailed questions on cybersecurity, or specic projects being undertaken
to address threats. The cyber market is ever-changing. New countermeasures should be considered as
cyber-attacks continue. In this new ongoing relationship, underwriters will ask more detailed questions
about controls to address specic threats related to recent attacks (e.g., SolarWinds breach). You should
expect to see the level of depth and scrutiny to continue to evolve. As such, it’s recommended to consider
the practices outlined in HICP as a starting place to prepare for underwriter questioning.
The threat of ransomware has now caused cyber insurance underwriters to consider numerous specic
countermeasures to address threats before issuing coverage, including:
• MFA for ofine and privileged access
• Email security that prevents harm from social engineering and/or malicious attachments and links
• Privileged access separation and management
• Air-gapped backups
• Continual vulnerability management
• Effective network segmentation of IoT and legacy devices
• EDR software
• Continual monitoring and threat response
• Drilling tabletop exercises
• Building and implementing downtime procedures for critical processes
• Frequency and level of detail of risk assessments
• Delivery of a continual risk management process
• Specic compliance standards (e.g., PCI-DSS)
What this means is that a relationship with an insurance provider is a good idea because it can help
provide continual assurance in these areas. It is no longer possible to transfer all cyber risk via insurance
because that presents too much risk to the insurance companies. However, working in partnership with
them can help augment your organization’s practices to address security requirements, while effectively
managing premium costs.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
130Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
When making the decision on coverage, consideration of the following is recommended:
110
• How much coverage will be offered?
• Will there be coverage from several providers based on escalating costs, or just one provider?
• What is the deductible based on the coverage?
• What other services does your organization provide to complement the policy?
• Based on a risk assessment of your organization, how much will a computer systems failure cost?
Many organizations that have had cyber-attacks were forced to pay tens of millions out of pocket
because their insurance premium did not cover the costs.
• Do sub-limits apply for social engineering, ransomware attacks, reputational loss, or business loss due
to system failures?
These services can include:
• Tabletop Exercise Facilitation: The broker can help facilitate services to conduct tabletop exercises to
determine readiness in case of an attack.
• Digital Forensics/Incident Response (DFIR) Panel: A list of pre-approved companies to choose from to
conduct DFIR services. However, unlike in the past, you will have to separately contract with these
rms to reserve services. This is because the demand for qualied DFIR professionals is so high that
unless you prepay for hours, you may not be able to get the professionals you need. You most likely
will not be able to add your rm of choice to this list.
• Legal Panel: A list of pre-approved law rms to use in case of an incident. Pay close attention to these
rms, who they have on staff and what experience that staff has in cybersecurity and healthcare.
• Security Risk Assessments: The broker can partner with (or provide themselves) security risk
assessment services to help determine areas for improvement, and most importantly, determine
what the premium should ideally be.
In summation, cyber insurance is an ongoing partnership used to continually improve your organization
and ensure that needed services are present and available.
What Should Your Cyber Insurance Policy Cover?
Consider coverage for:
• Data breaches (like incidents involving theft of personal information)
• Cyber-attacks on your data held by vendors and other third-parties
• Cyber-attacks (like breaches of your network)
• Cyber-attacks that occur anywhere in the world (not only in the United States)
• Cyber-attacks determined to be nation-state attackers
• Cyber-attacks aided by insiders both intentional and unintentional
• Cyber-attacks that lead to extortion (ransomware attacks)
• Terrorist acts
• Cyber warfare
110 “Cyber Insurance,” Federal Trade Commission (FTC) (Accessed June 1, 2022), https://www.ftc.gov/tips-advice/
business-center/small-businesses/cybersecurity/cyber-insurance.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
131Technical Volume 2: Cybersecurity Practices for Medium and Large Healthcare Organizations |
Also, consider whether your cyber insurance provider will:
• Defend you in a lawsuit or regulatory investigation (look for “duty to defend” wording)
• Provide coverage in excess of any other applicable insurance you have
• Offer a breach hotline that’s available 24x7x365
• Provide access to third-party breach specialists, including forensics, independent legal counsel
working on your behalf, not the cyber insurance provider, and incident remediation rms
• Require you to use specic vendors for IR
• Provide coverage for notication costs including printing, mailing, phone centers, and PR assistance
• Loss of business coverage or revenue
Key Mitigated Threats
1. Social engineering
2. Ransomware attacks
3. Loss or theft of equipment or data
4. Insider, accidental or malicious data loss
5. Attacks against network connected medical devices that may affect patient safety
Suggested Metrics
• Number of policies reviewed over a specied timeframe, suggested every three years. The goal is to
establish a standard practice to review policies and to monitor compliance with this standard.
• Number of workforce members who review and sign off after reading policies over a specied timeframe,
suggested yearly. The goal is to establish a standard practice for workforce members to review
applicable policies and attest to the review, and for your organization to monitor compliance with
this standard.
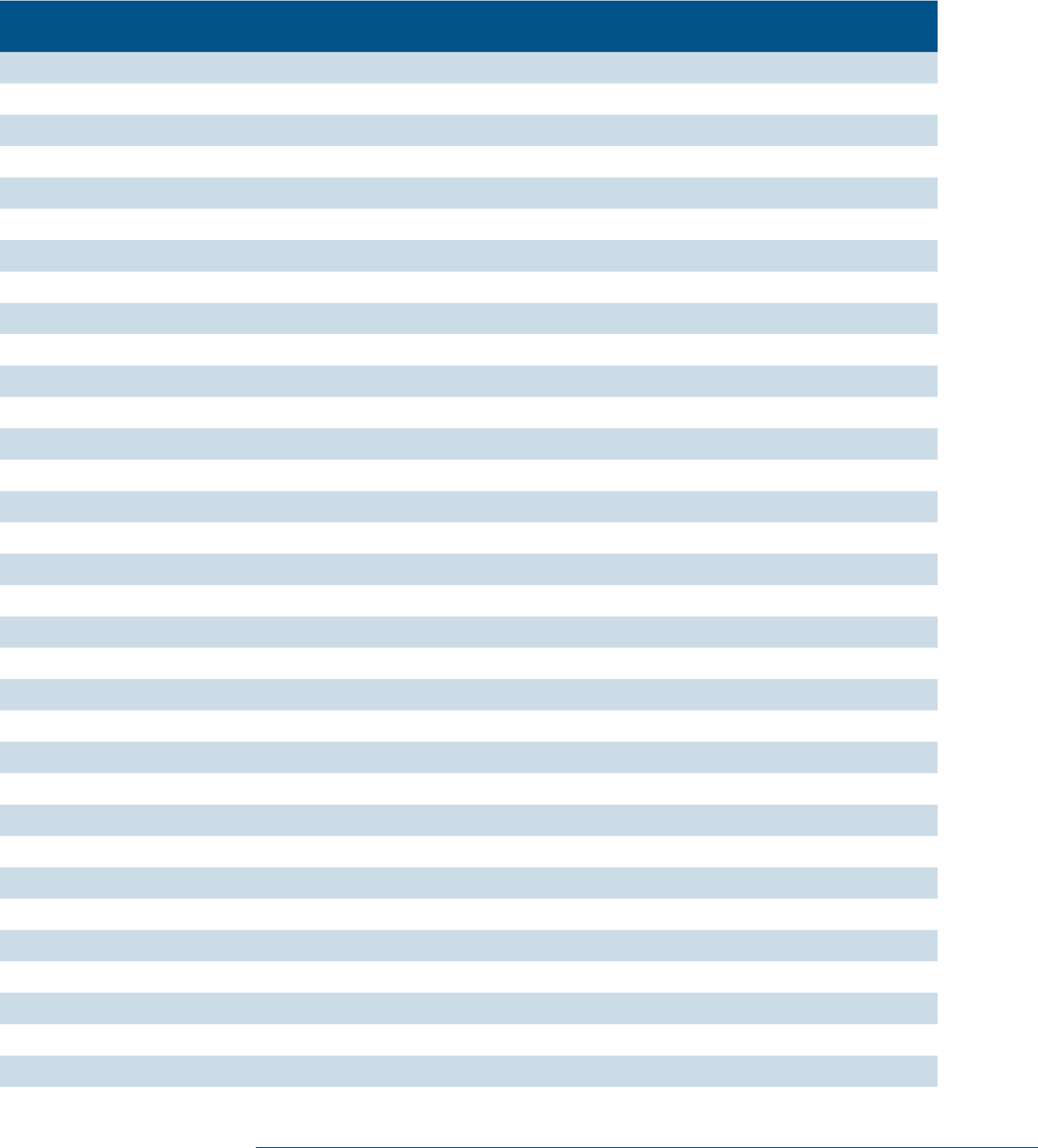
132Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Appendix A: Acronyms and Abbreviaons
Table 17. Acronyms and Abbreviations
Acronym/Abbreviaon Denion
ABAC Attribute Based Access Control
AHIP America’s Health Insurance Plans
ASL Assistant Secretary for Legislation
ASPR Administration for Strategic Preparedness and Response
ASTM American Society for Testing and Materials
ATT&CK Adversarial Tactics, Techniques & Common Knowledge
AV Antivirus
BYOD Bring Your Own Device
CAB Change Advisory Board
C2 Command and Control
CEO Chief Executive Ofcer
CHIO Chief Health Information Ofcer
CIO Chief Information Ofcer
CIRT Cybersecurity Incident Response Team
CISO Chief Information Security Ofcer
CISSP Certied Information Security Systems Professional
CMS Centers for Medicare and Medicaid
CNSSI Committee on National Security Systems Instruction
COO Chief Operations Ofcer
CSA Cybersecurity Act
CT Computed Tomography
CVSS Common Vulnerability Scoring System
DCC Distributed Checksum Clearinghouse
DEP Device Enrollment Program
DICOM Digital Imaging and Communications in Medicine
DKIM Domain Key Identied Mail
DLP Data Loss Prevention
DMARC Domain-based Message Authentication Reporting and Conformance
DMZ Demilitarized Zone
DNS Domain Name System
DNSRBL Domain Name System Real-time Blackhole List
DoD Department of Defense
DOS Denial of Service
DRP Disaster Recovery Plan

Appendix A: Acronyms and Abbreviations
133Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Acronym/Abbreviaon Denion
DSM Direct Secure Messaging
EDR Endpoint Detection and Response
EHR Electronic Health Record
EMR Electronic Medical Record
ePHI Electronic Protected Health Information
ERP Enterprise Resource Planning
FDA Food and Drug Administration
FERPA Family Educational Rights and Privacy Act
FIPS Federal Information Processing Standards
FTP File Transfer Protocol
GDPR General Data Protection Regulation
GINA Genetic Information Nondiscrimination Act
HCIC Health Care Industry Cybersecurity
HDO Health Delivery Organization
HIDS Host Based Intrusion Detection Systems
HIPAA Health Insurance Portability and Accountability Act
HIPS Host Based Intrusion Prevention Systems
HIT Health Information Technology
HITECH Health Information Technology Economic and Clinical Health Act
HL7 Health Level Seven
HMO Health Maintenance Organization
HPH Health Care and Public Health
HR Human Resources
HRSA Health Resources and Services Administration
HTTP Hypertext Transfer Protocol
HTTPS Hypertext Transfer Protocol Secure
IA Information Assurance
IAM Identity and Access Management
IBM International Business Machines
ICMP Internet Control Message Protocol
ICU Intensive Care Unit
IDS Intrusion Detection System
IHI Individually Identiable Health Information
INFOSEC Information Security
IOC Indicator of Compromise
IoT Internet of Things
IP Intellectual Property or Internet Protocol
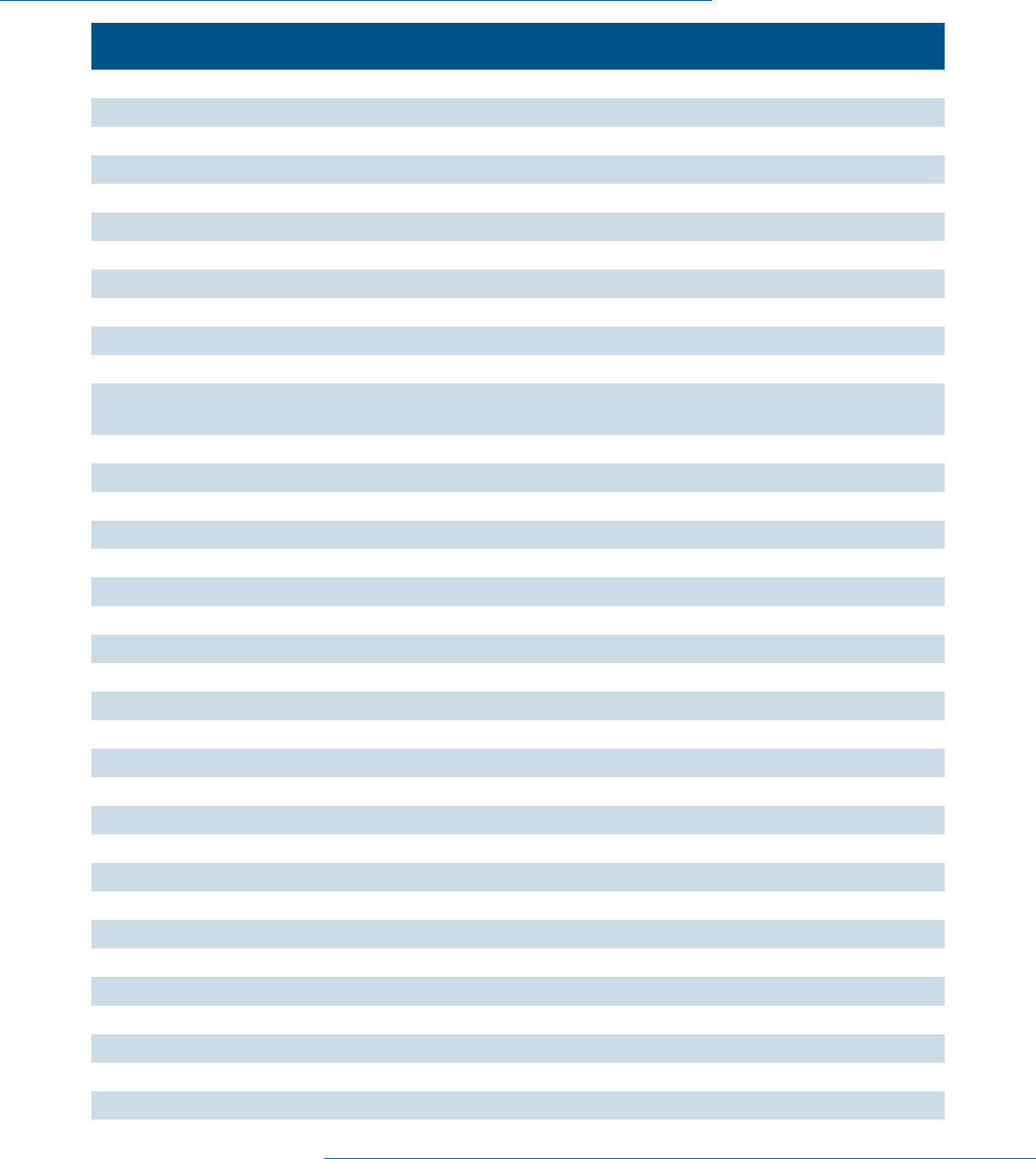
Appendix A: Acronyms and Abbreviations
134Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Acronym/Abbreviaon Denion
IPS Intrusion Prevention Systems
ISAC Information Sharing and Analysis Center
ISAO Information Sharing and Analysis Organization
IT Information Technology
ITIL Information Technology Infrastructure Library
ITAM Information Technology Asset Management
LAN Local Area Network
LANMAN Local Area Network Manager
LIS Laboratory Information Systems
LLC Limited Liability Corporation
MAC Media Access Control
MACRA Medicare access and the Children’s Health Insurance Program
Reauthorization Act
MDM Mobile Device Management
MDS2 Manufacturer Disclosure Statement for Medical Device Security
MFA Multi-Factor Authentication
MIB Management Information Base
MITRE The MITRE Corporation
MRI Magnetic Resonance Imaging
NAC Network Access Control
NCI National Cancer Institute
NIST National Institute of Standards and Technology
NNCOE NIST National Cybersecurity Center of Excellence
NVD National Vulnerability Database
OCIO Ofce of the Chief Information Ofcer
OCR Ofce for Civil Rights
ONC Ofce of the National Coordinator (for Healthcare Technology)
OS Operating System
PCI-DSS Payment Card Industry Data Security Standard
PCS Patient Care Service
PHI Protected
Health Information
PII Personally Identiable Information
RADIUS Remote Authentication Dial-In User Service (RADIUS)
RBAC Rule Based Access Control
RDP Remote Desktop Protocol
ROM Read Only Memory
SAMHSA Substance Abuse and Mental Health Services Administration

Appendix A: Acronyms and Abbreviations
135Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Acronym/Abbreviaon Denion
SBOM Software Bill of Materials
SIEM Security Incident and Event Management
SMB Server Message Block
SME Subject Matter Expert
S/MIME Secure Multi-Purpose Internet Mail Extensions
SMTP Simple Mail Transfer Protocol
SSH Secure Shell
SSN Social Security Number
SSO Single Sign On
STIX Structure Threat Information eXpression
SVP Senior Vice President
TAXII Trusted Automated eXchange of Indicator Information
TLS Transport Layer Security
TXT Text
UBA User Behavior Analytics
UPnP Universal Plug and Play
URL Uniform Resource Locator
US-CERT United States Computer Emergency Readiness Team
USB Universal Serial Bus
VAR Value Added Reseller
VP Vice President
VPN Virtual Private Network
WAN Wide Area Network
136Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Appendix B: References
“4.1.9 Federal Information Security Management Act,” NIH, https://grants.nih.gov/grants/policy/nihgps/
html5/section_4/4.1.9_federal_information_security_management_act.htm.
2020 Data Breach Investigations Report (DBIR), Verizon, 2020, https://www.verizon.com/business/
resources/reports/dbir/2020/.
“2021 Data Breach Investigations Report,” Verizon, 2021, https://www.verizon.com/business/resources/
reports/2021/2021-data-breach-investigations-report.pdf.
Adam Sedgewick, Murugiah Souppaya, and Karen Scarfone, NIST Special Publication 800-167: Guide to
Application Whitelisting, National Institutes of Science and Technology (NIST), October 2015, http://
nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.800-167.pdf.
“Attribute Based Access Control,” NIST Computer Security Resource Center, February 13, 2013, https://
csrc.nist.gov/Projects/Attribute-Based-Access-Control.
“Bad Practices,” CISA (Accessed June 2, 2022), https://www.cisa.gov/BadPractices.
Bill Mathers et al., “Implementing Least-Privilege Administrative Models,” Microsoft Windows IT Pro
Center, May 31, 2017, https://docs.microsoft.com/en-us/windows-server/identity/ad- ds/plan/
security-best-practices/implementing-least-privilege-administrative-models.
Brandon Vigliarolo, “Report: The IT Response to WannaCry,” TechRepublic, July 25, 2017, https://www.
techrepublic.com/article/report-the-it-response-to-wannacry/.
“California Consumer Privacy Act (CCPA),” State of California Department of Justice, https://oag.ca.gov/
privacy/ccpa.
“CIS Benchmarks,” Center for Information Security, September 24, 2018, https://www.cisecurity.org/cis-
benchmarks/.
“CIS Control 1: Inventory and Control of Hardware Assets,” Center for Information Security Controls,d
September 24, 2018, https://www.cisecurity.org/controls/inventory-and-control-of-hardware-
assets/.
“CIS Control 2: Inventory of Authorized and Unauthorized Software,” Center for Internet Security
Controls, September 24, 2018, https://www.cisecurity.org/controls/inventory-of-authorized-and-
unauthorized-software/.
“CIS Control 5: Secure Congurations for Hardware and Software on Mobile Devices, Laptops,
Workstations and Servers,” Center for Information Security Controls, September 24, 2018. https://
www.cisecurity.org/controls/secure-conguration-for-hardware-and-software-on-mobile-devices-
laptops-workstations-and-servers/.
“CIS Critical Security Control 12: Network Infrastructure Management,” Center for Information Security
Controls, June 2, 2022, https://www.cisecurity.org/controls/boundary-defense/.
“CIS Critical Security Control 18: Penetration Testing,” Center for Internet Security, September 24, 2018,
https://www.cisecurity.org/controls/penetration-testing.
“CISA Tabletop Exercises Packages,” CISA, May 31, 2022, https://www.cisa.gov/cisa-tabletop-exercises-
packages.
“CommHIT Information Sharing & Analysis Centers (ISACs),” CommunityHealth IT, May 31, 2022,
https://www.communityhealthit.org/isacs/.

Appendix B: References
137Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
“Common Platform Enumerations (CPE),” NIST National Vulnerability Database (NVD), June 2, 2022,
https://nvd.nist.gov/products/cpe/search.
“Common Vulnerability Scoring System version 3.1: Specication Document,” FIRST, June 2, 2022,
https://www.rst.org/cvss/specication-document.
“Common Weakness Enumeration (CWE),” MITRE, June 2, 2022, https://cwe.mitre.org/.
“Controlling Root Access,” Redhat Customer Portal, September 24, 2018, https://access.redhat.com/
documentation/en-us/red_hat_enterprise_linux/7/html/security_guide/sec- controlling_root_access.
“Cyber Hygiene Services,” CISA, June 2, 2022, https://www.cisa.gov/cyber-hygiene-services.
“Cyber Insurance,” Federal Trade Commission (FTC), June 1, 2022, https://www.ftc.gov/tips-advice/
business-center/small-businesses/cybersecurity/cyber-insurance.
“Cybersecurity,” FDA, https://www.fda.gov/medical-devices/digital-health-center-excellence/
cybersecurity.
Cybersecurity Framework Version 1.1, NIST, April 2018, https://www.nist.gov/cyberframework/
framework.
“Cybersecurity Framework,” NIST, June 1, 2022, https://www.nist.gov/cyberframework.
“Cyber Storm: Securing Cyber Space,” CISA, May 26, 2022, https://www.cisa.gov/cyber-storm-securing-
cyber-space.
David Swift, Successful SIEM and Log Management Strategies for Audit and Compliance, The SANS Institute,
November 9, 2010, https://www.sans.org/reading-room/whitepapers/auditing/successful-siem-log-
management-strategies-audit-compliance-33528.
“DEP Guide,” Apple, October 2015, https://www.apple.com/business/site/docs/DEP_Guide.pdf.
“DHS Cyber Tabletop Exercise (TTX) for the Healthcare Industry [Exercise Materials],” Homeland
Security Digital Library, 2013, https://www.hsdl.org/?abstract&did=789781.
“Does the Security Rule allow for sending electronic PHI (e-PHI) in an email over the Interent? If so,
what protections must be applied?,” HHS OCR. July 26, 2013, https://www.hhs.gov/hipaa/for-
professionals/faq/2006/does-the-security-rule-allow-for-sending-electronic-phi-in-an-email/index.
html.
Erika McCallister, Tim Grance, and Karen Scarfone, NIST Special Publication 800-122: Guide to Protecting
the Condentiality of Personally Identiable Information (PII), April 2010, https://nvlpubs.nist.gov/
nistpubs/Legacy/SP/nistspecialpublication800-122.pdf.
Erik Decker, et al., “Toolkit for Developing and Identity and Access Management (IAM) Program,”
EDUCAUSE May 7, 2013, https://library.educause.edu/resources/2013/5/toolkit-for-developing-an-
identity-and-access-management-iam-program.
Executive Order No. 14028, May 12, 2012, https://www.whitehouse.gov/brieng-room/presidential-
actions/2021/05/12/executive-order-on-improving-the-nations-cybersecurity/.
“Fact Sheet: SAMHSA 42 CFR Part 2 Revised Rule,” SAMHSA, https://www.samhsa.gov/newsroom/
press-announcements/202007131330.
“Family Educational Rights and Privacy Act (FERPA),” US Department of Education, https://www2.
ed.gov/policy/gen/guid/fpco/ferpa/index.html.
“Field Ofces,” FBI. May 31, 2022, https://www.fbi.gov/contact-us/eld-ofces.
Appendix B: References
138Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
“Fraud & Abuse Laws,” HHS Ofce of Inspector General, https://oig.hhs.gov/compliance/physician-
education/fraud-abuse-laws/#:~:text=The%20Physician%20Self%2DReferral%20Law%2C%20
commonly%20referred%20to%20as%20the,relationship%2C%20unless%20an%20exception%20
applies.
Gavin O’Brien et al., NIST Special Publication 1800-8: Securing Wireless Infusion Pumps In Healthcare
Delivery Organizations, NIST. August 2018. https://www.nccoe.nist.gov/sites/default/les/library/
sp1800/hit-wip-nist-sp1800-8.pdf.
“General Data Protection Regulation: GDPR,” Intersoft Consulting, https://gdpr-info.eu/.
“Genetic Information,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/special-topics/genetic-
information/index.html.
Gordon Fraser, “A Practical Example of Incident Response to a Network Based Attack,” The SANS
Institute. August 16, 2017. https://www.sans.org/white-papers/37920/.
“Gramm-Leach-Bliley Act,” FTC, https://www.ftc.gov/business-guidance/privacy-security/gramm-leach-
bliley-act.
Health-ISAC (H-ISAC), https://h-isac.org/.
Healthcare Industry Cybersecurity Workforce Guide: Recruiting and Retaining Skilled Cybersecurity
Talent, Healthcare & Public Health Sector Coordinating Council (HSCC). June 2019. https://
healthsectorcouncil.org/workforce-guide/.
Health Industry Cybersecurity — Matrix of Information Sharing Organizations (HIC-MISO), HSCC. Accessed
May 31, 2022. https://healthsectorcouncil.org/hic-miso/.
Health Industry Cybersecurity Supply Chain Risk Management Guide (HIC-SCRiM), Healthcare & Public
Health Sector Coordinating Councils (HSCC). September 2020. https://healthsectorcouncil.org/hic-
scrim-v2/.
“Health Sector Cybersecurity Coordination Center (HC3),” HHS.gov. March 31, 2022. https://www.hhs.
gov/about/agencies/asa/ocio/hc3/products/index.html#sector-alerts.
“HITECH Act Enforcement Interim Final Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/
special-topics/hitech-act-enforcement-interim-nal-rule/index.html.
“ICS-CERT Advisories,” CISA. June 2, 2022. https://www.cisa.gov/uscert/ics/advisories.
IEC 80001-1:2021: Application of risk management for IT-networks incorporating medical devices — Part 1:
Safety, effectiveness and security in the implementation and use of connected medical devices or connected
health software, ISO, September 2021, https://www.iso.org/standard/72026.html.
“Incident Response Training,” CISA. May 26, 2022. https://www.cisa.gov/incident-response-training#.
ISAO Standards Organization, https://www.isao.org/.
KC Cross, Denise Vangel, and Meera Krishna, “Use DMARC to Validate Email in Ofce 365,” Microsoft
TechNet. October 8, 2017. https://technet.microsoft.com/en- us/library/mt734386(v=exchg.150).
aspx.
KC Cross and Denise Vangel, “Congure Your Spam Filter Policies,” Microsoft TechNet. December 13,
2017. https://technet.microsoft.com/en- us/library/jj200684(v=exchg.150).aspx.
Keith Ferrazzi, “7 Ways to Improve Employee Development Programs,” Harvard Business Review. July
31, 2015. https://hbr.org/2015/07/7-ways-to-improve-employee-development-programs.
Appendix B: References
139Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
Kevin Stine, Stephen Quinn, and Robert Gardner, NISTIR 8286: Integrating Cybersecurity and Enterprise Risk
Management (ERM), NIST. October 2020. https://csrc.nist.gov/publications/detail/nistir/8286/nal.
“Learn the Process,” The Joint Commission, https://www.jointcommission.org/accreditation-and-
certication/become-accredited/learn-the-process/.
“MACRA,” Centers for Medicare and Medicaid Services (CMS), https://www.cms.gov/Medicare/Quality-
Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/
MACRA-MIPS-and-APMs#:~:text=The%20Medicare%20Access%20and%20CHIP,clinicians%20
for%20value%20over%20volume.
Manufacturer Disclosure Statement for Medical Device Security, NEMA. October 28, 2019. https://www.
nema.org/Standards/view/Manufacturer-Disclosure-Statement-for-Medical-Device-Security.
Medical Device and Health IT Joint Security Plan, HSCC. January 2019. https://healthsectorcouncil.org/the-
joint-security-plan/.
Michael Kassner, “Anatomy of the Target data breach: Missed opportunities and lessons learned,” ZDNet
February 2, 2015. https://www.zdnet.com/article/anatomy-of-the-target-data-breach-missed-
opportunities-and-lessons-learned/.
Michael Stone et al., NIST Special Publication 1800-5b: IT Asset Management, NIST. October 2015. https://
nccoe.nist.gov/sites/default/les/library/sp1800/fs-itam-nist-sp1800-5b-draft.pdf.
“Minimum Acceptable Risk Standards for Exchanges (MARS-E) 2.0,” HHS Guidance Portal, https://www.
hhs.gov/guidance/document/minimum-acceptable-risk-standards-exchanges-mars-e-20.
MITRE ATT&CK®. May 26, 2022. https://attack.mitre.org/.
Model Contract-language for Medtech Cybersecurity (MC2), Healthcare & Public Health Sector Coordinating
Councils (HSCC). March 2022. https://healthsectorcouncil.org/model-contract-language-for-
medtech-cybersecurity-mc2/.
Murthy Raju, “Using RBL and DCC for Spam Protection,” Linux.com. June 14, 2007. https://www.linux.
com/news/using-rbl-and-dcc-spam-protection.
“National Vulnerability Database,” NIST. June 2, 2022. https://nvd.nist.gov/.
“National Vulnerability Database: CVSS,” NIST. Accessed September 24, 2018. https://nvd.nist.gov/vuln-
metrics/cvss.
“NIST Risk Management Framework: SP 800-53 Controls and SP 800-53B Control Baselines Resources
for Implementers,” NIST. May 26, 2022. https://csrc.nist.gov/Projects/risk-management/sp800-53-
controls.
“NTIA Software Component Transparency,” National Telecommunications and Information
Administration (NTIA) April 28, 2021. https://www.ntia.doc.gov/SoftwareTransparency.
NIST Special Publication NIST SP 800-66r2 ipd Implementing the Health Insurance Portability and
Accountability Act (HIPAA) Security Rule: A Cybersecurity Resource Guide, NIST. July 2022. https://
nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.SP.800-66r2.ipd.pdf.
NIST Special Publication 1800-24: Securing Picture Archiving and Communication Systems (PACS):
Cybersecurity for the Healthcare Sector, NIST, December 2020, https://nvlpubs.nist.gov/nistpubs/
SpecialPublications/NIST.SP.1800-24.pdf.
ONC’s Cures Act Final Rule, https://www.healthit.gov/curesrule/.
Appendix B: References
140Technical Volume 2: Cybersecurity Practices for Medium and Large Health Care Organizations |
“OWASP Top 10 - 2017: Ten Most Critical Web Application Security Risks,” OWASP, 2017, https://raw.
githubusercontent.com/OWASP/Top10/master/2017/OWASP%20Top%2010-2017%20(en).pdf.
Patrick Kral, “The Incident Handlers Handbook,” The SANS Institute, February 21, 2012, https://www.
sans.org/white-papers/33901/.
Paul A. Grassi, Michael E. Garcia, and James L. Fenton, NIST Special Publication 800-63: Digital Identity
Guidelines, NIST (June 2017), https://pages.nist.gov/800-63-3/sp800-63-3.html.
Paul A. Grassi et al., NIST Special Publication 800-63B: Digital Identity Guidelines: Authentication and
Lifecycle Management, NIST, June 2017, https://nvlpubs.nist.gov/nistpubs/SpecialPublications/NIST.
SP.800-63b.pdf.
Paul Cichonski et al., NIST Special Publication 800-61r2: Computer Security Incident Handling Guide, NIST
August 2012, https://nvlpubs.nist.gov/nistpubs/specialpublications/nist.sp.800-61r2.pdf.
“PCI DSS v4.0 Resource Hub,” PCI Security Standards Council, https://www.pcisecuritystandards.org/.
Peter Czanik and BalaBit, “The 6 Categories of Critical Log Information,” S!NS Technology Security
Laboratory, last modied 2013, February 4, 2018, https://www.sans.edu/cyber-research/security-
laboratory/article/sixtoplogcategories.
Postmarket Management of Cybersecurity in Medical Devices, Food and Drug Administration (FDA) October
1, 2018, https://fda.gov/regulatory-information/search-fda-guidance-documents/postmarket-
management-cybersecurity-medical-devices.
“Principles and Practices for Medical Device Cybersecurity,” IMDRF Medical Device Cybersecurity
Working Group, March 2020, https://www.imdrf.org/sites/default/les/docs/imdrf/nal/technical/
imdrf-tech-200318-pp-mdc-n60.pdf.
“Ransomware Guide,” MS-ISAC and CISA, September 2020, https://www.cisa.gov/sites/default/les/
publications/CISA_MS-ISAC_Ransomware%20Guide_S508C.pdf.
“Registration Requirements,” SAMHSA, https://www.samhsa.gov/grants/applying/registration-
requirements.
“SAFER Guide: Contingency Planning,” ONC HealthIT, July 2016, https://www.healthit.gov/sites/default/
les/safer/guides/safer_contingency_planning.pdf.
“Security Risk Assessment Tool,” Ofce of the National Coordinator for Health Information Technology
(ONC), February 15, 2022, https://www.healthit.gov/topic/privacy-security-and-hipaa/security-risk-
assessment-tool.
“Security Rule Guidance Material: Guidance on Risk Analysis,” HHS.gov, https://www.hhs.gov/hipaa/for-
professionals/security/guidance/guidance-risk-analysis/index.html.
“Security Technical Implementation Guides (STIGs),” Information Assurance Support Environment
(IASE), September 24, 2018, https://public.cyber.mil/stigs/.
SP 800-30 Rev. 1; Guide for Conducting Risk Assessments, NIST, September 2012, https://csrc.nist.gov/
publications/detail/sp/800-30/rev-1/nal.
StopRansomware.gov, CISA, May 31, 2022, https://www.cisa.gov/stopransomware.
The Association of Electrical Equipment and Medical Imaging Manufacturers (MDS2) form HN 1-203, rev.2019,
NEMA, 2019, https://www.nema.org/Standards/ComplimentaryDocuments/MDS2-Worksheet.xlsx.
“The HIPAA Privacy Rule,” HHS.gov, https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
